Translate this page into:
Awareness among health care professionals regarding interrelationship between diabetes mellitus and periodontal diseases: A step towards interprofessional collaborative practice
-
Received: ,
Accepted: ,
How to cite this article: Bains VK, Chandra H, Jamaluddin K, Bains R. Awareness among health care professionals regarding interrelationship between diabetes mellitus and periodontal diseases: A step towards interprofessional collaborative practice. Asian J Oral Health Allied Sci 2020;10:10.
Abstract
Objectives:
The objective of the study was to assess the level of awareness among health care professionals regarding interrelationships between diabetes mellitus (DM) and periodontal diseases.
Material and Methods:
A self-administered, structured questionnaire based on scientific literature, and practice was distributed among 100 non-oral health care professionals (NOHCP) and 100 oral-health care professionals (OHCP) for assessment of their awareness regarding DM and periodontitis interrelationship (DPI). One hundred fifty-four (154) participants who responded and returned the questionnaire were interviewed to avoid any obscurity pertinent to the questionnaire and to obtain their suggestions or recommendations. Twenty-seven participant’s questionnaires were excluded due to non-availability for interview to clarify the information given. Responses of 127 participants were finally statistically analyzed.
Results:
Almost 79% of OHCPs were aware of the DPI. About 9% of OHCPs did not agree with DPI and 11% of them were “unaware” about the DPI. Similarly, about 65% of NOHCPs were aware of the DPI. About 15% of OHCPs did not agree with DPI and 19% of OHCPs were “unaware” about the DPI.
Conclusion:
A limited awareness was observed among health care professionals participating in the present study for DPI, highlighting a gap of knowledge, attitude, and practice for DPI, which was higher among NOHCP than OHCPs.
Keywords
Diabetes mellitus
Interprofessional interrelationship
Periodontal disease
INTRODUCTION
Worldwide, 50% of 425 million diabetic adults are undiagnosed, and in spite of advances in the development of new therapies, there is a substantial burden of diabetes on the health care system.[1] Complications resulting from uncontrolled diabetes can lead to significant morbidity as well as premature death. India has witnessed a rapidly exploding epidemic of diabetes mellitus (DM).[2,3] It is critical for all health care professionals to assess individuals carefully to identify those who are at risk for DM, to identify the disease in undiagnosed persons, and to assist those with DM in achieving optimum health. Oral health care professionals (OHCP), ophthalmologists, physicians, endocrinologists, diabetes educators, and family care providers need to support the efforts and reinforce key concepts of DM regularly to help diabetic patients achieve successful health outcomes. An interprofessional collaborative practice (ICP) approach among a variety of health care providers is recommended to support diabetes awareness, prevention, and management.[4,5]
Periodontitis, a chronic periodontal disease, is a bacterial-induced, local, chronic inflammatory disease of the supporting tissues of teeth (i.e., periodontal tissues). This leads to gingival inflammation, destruction of periodontal tissues, loss of alveolar bone, and eventual exfoliation of teeth in severe cases.[6] Due to induced or perpetuated elevated systemic chronic inflammatory state, which is reflected by increased serum CRP, IL-6, and fibrinogen levels, chronic Gram-negative periodontal infections may result in increased insulin resistance and poor glycemic control. Emerging evidences have shown that oral health may influence systemic health, and there may be a bi-directional relationship between periodontal disease and DM.[7]
The interrelationship between periodontal disease and DM provides an example of a cyclical association, whereby a systemic disease predisposes the individual to oral infections, and once the oral infection is established, it exacerbates the systemic disease.[8] There is a need for greater collaboration and increased numbers of cross-referrals between medical and dental professionals. However, gap in knowledge for understanding biologic plausibility along-with limited published meta-analysis of randomized clinical trials, due to heterogeneous study design and numerous confounding factors affecting these two chronic diseases, that is, DM and periodontitis,[9] medical professionals are reluctant to emphasize on considering oral health examination and periodontal therapy in the standard treatment protocol for the management of diabetes mellitus (DM).
As periodontal disease is a modifiable risk factor for DM,[10] it should be treated even if direct causal evidence does not yet exist. However, it has been observed that periodontal health although recognized as an important part of overall health and well-being but is often overlooked as an important component of many interprofessional collaborative approach of care. Many knowledge, attitude, and practice (KAP) studies have been conducted in the past for assessment of perception of the possible interrelationship between oral and systemic health among medical doctors,[11-18] as well as among patients and general population,[19-22] however, to the best of our knowledge no study have been published so for to understand and compare awareness of OHCPs and NOCHPs for KAP of health care professionals. Thus, the present study was designed with the aim to assess level of knowledge among health care professionals regarding interrelationships between DM and periodontal diseases; to assess the gap in understanding and difficulty in implementing oral health examination and periodontal therapy in the standard treatment protocol for the management of DM.
MATERIAL AND METHODS
A present cross-sectional study was conducted in the Department of Periodontology, Saraswati Dental College, Lucknow, in collaboration with the Department of Hospital Administration, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India. The studied population consisted of the health care professionals practicing in Lucknow. All eligible subjects were thoroughly informed of the nature, potential risks, and benefits of their participation in the study. For the study, a self-administered, structured, questionnaire based on scientific literature and practice were distributed among 200 health care professionals (100-NOHCP and 100-OHCP) for assessment of their awareness regarding DM and periodontitis interrelationship (DPI) during August 2017 to October 2017. Non-oral health care professionals (NOHCP) were medical consultants (Physicians) who were practicing in the management of DM. OHCP were practicing dental surgeons having a minimum degree of Bachelor of Dental Sciences or above in the city. The questionnaire and study protocol were approved by SDC-Institutional Research and Development Committee. A preliminary study of the questionnaire was conducted among 25 health care professionals to validate the survey, and the questions, which were incomprehensible or ambiguous, were removed from the final survey.
Questionnaire
The study was designed to keep the anonymity of the responders in mind, and no identification markers such as name or e-mail address were inquired. Both convenience sampling (researchers themselves contacted OHCP and NOHCP to participate in the study) and snowball sampling (the participating OHCP and NOCHP were asked to forward the questionnaire to their colleagues) were used. The first section of the form was a declaration stating that participation in this survey was voluntary, data will be used for this research only and results will be kept confidential. The second section of the questionnaire consisted of 24 questions that were divided into three sections to assess various aspects of awareness from “knowledge” (first 13 questions), “attitude” (next 8 questions), and “practice” (last 3 questions). All the questions have any of three scores; Score 1: “Agreed or Yes,” Score 2: “Disagree or No,” and Score 3: “Unaware or No idea”
Among 200 distributed questionnaires, 154 questionnaires were returned. Participants who responded and returned the questionnaire were interviewed to avoid any obscurity pertinent to the questionnaire, and to obtain their suggestions or recommendations. A study flow chart explaining the methodology is shown in Figure 1.
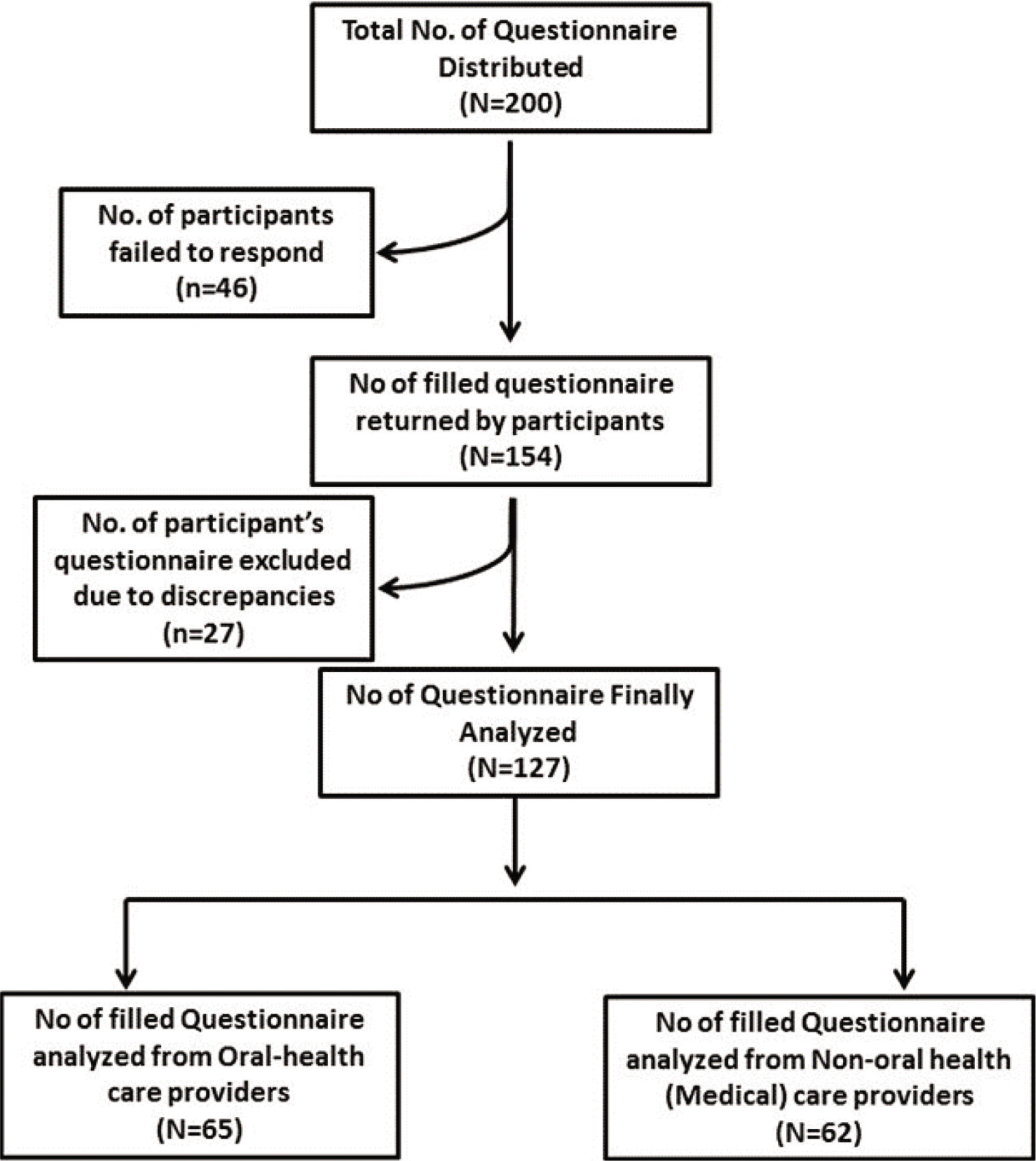
- Flow chart showing study design.
Statistical analysis
Categorical variables were presented in number and percentage. Qualitative variables were compared using Chi-square test/Fisher’s exact test as appropriate. P < 0.05 will be considered statistically significant. The data were entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for the Social Sciences version 21.0.
RESULTS
Out of 200 questionnaires distributed, only 154 participants returned their questionnaire, among them, 27 were excluded for discrepancies, such as incomplete information, choosing more than one option, or casually choosing only one type of option among the entire study, or could not be contacted for one-to-one interview to resolve these inconsistencies. Finally, 127 responses of health care professionals were analyzed, among whom 65 were OHCPs, and 62 belongs to the NOHCPs (physicians) managing DM in their practices.
Out of total of 127 participants, 65 (52.18%) were OHCPs and 62 (48.82%) were NOHCPs. Among 24 questions in the questionnaire for the present study, almost 79% of OHCPs were “Aware” of the DM-periodontitis interrelationship (DPI), in comparison to 65% of NOHCPs. About 9% of OHCPs and 15% of NOHCPs responded against DPI. Further, 19% of NOCPs were “unaware” about DPI in comparison to 11% of OHCPs.
Results indicated that 83% OHCPs were having “knowledge” of DPI in contrast to 69% of NOHCPs, and 22% of NOHCPs reported “no-idea” about DPI in contrast to 13% of OHCPs. Almost similar trends of results were observed for “attitude” toward DPI, also. For “practice” of DPI, however, the level of response from both OHCPs and NOHCPs was non-significantly different, and overall was less than 60% for both OHCPs and NOCHPs and was about 56% versus 51% for OHCPs versus NOHCPs, respectively [Table 1].
| Questions | Agree/Yes | Disagree/No | No Idea | χ2 | P-value | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OHCP | NOHCP | OHCP | NOHCP | OHCP | NOHCP | ||||||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||||||||||||||
| By 2020, there will be approximately 250 million people affected by T2DM | 44 | 67.69 | 49 | 79.03 | 5 | 7.69 | 1 | 1.61 | 16 | 24.62 | 12 | 19.35 | 3.438 | 0.179 | |||||||||||
| In India, it is estimated that 80 million by the year 2030 will be suffering from T2DM | 47 | 72.31 | 48 | 77.42 | 3 | 4.62 | 2 | 3.23 | 15 | 23.08 | 12 | 19.35 | 0.473 | 0.789 | |||||||||||
| Are you aware that uncontrolled or poorly controlled diabetes is associated with increased susceptibility to oral infections, including periodontitis? | 63 | 96.92 | 54 | 87.10 | 2 | 3.08 | 6 | 9.68 | 0 | 0.00 | 2 | 3.23 | 4.624 | 0.099 | |||||||||||
| Patients with poorly controlled diabetes have pronounced gingival sessile or pedunculated proliferations or polyp, severe gingivitis, diminished salivary flow, burning mouth or tongue, xerostomia, higher incidence of dental caries. | 64 | 98.46 | 48 | 77.42 | 1 | 1.54 | 5 | 8.06 | 0 | 0.00 | 9 | 14.52 | 13.889 | 0.001* | |||||||||||
| Periodontal disease is the sixth complication of diabetes. | 53 | 81.54 | 23 | 37.10 | 1 | 1.54 | 7 | 11.29 | 11 | 16.92 | 32 | 51.61 | 12.831 | 0.002 | |||||||||||
| Are you aware that periodontal diseases are known to impair systemic health in susceptible individuals with metabolic disorders, atherosclerosis, cardiovascular, and rheumatoid arthritis, as well as aspiration pneumonia? | 56 | 86.15 | 43 | 69.35 | 1 | 1.54 | 7 | 11.29 | 8 | 12.31 | 12 | 19.35 | 6.940 | 0.031 | |||||||||||
| Severe periodontitis is associated with poor glycemic induced control and exacerbated diabetes-induced hyperglycemia, and increases chances of diabetic complications. | 54 | 83.08 | 39 | 62.90 | 1 | 1.54 | 7 | 11.29 | 10 | 15.38 | 16 | 25.81 | 8.238 | 0.016 | |||||||||||
| Individuals with diabetes tend to have a higher prevalence and more severe periodontitis than non-diabetics. | 55 | 84.62 | 48 | 77.42 | 0 | 0.00 | 9 | 14.52 | 10 | 15.38 | 5 | 8.06 | 11.078 | 0.004 | |||||||||||
| Diabetes mellitus and chronic periodontitis are common diseases in adults in the world population. | 62 | 95.38 | 52 | 83.87 | 3 | 4.62 | 6 | 9.68 | 0 | 0.00 | 4 | 6.45 | 5.810 | 0.054 | |||||||||||
| Both chronic periodontitis and diabetes mellitus can modulate host immune responses, such as up-regulation of inflammation. | 57 | 87.69 | 47 | 75.81 | 1 | 1.54 | 4 | 6.45 | 7 | 10.77 | 11 | 17.74 | 3.582 | 0.167 | |||||||||||
| Do you know that periodontal diseases are commonly regarded as “silent diseases” since patients often live with no or few symptoms, that is, bleeding and swelling from gums without sense of pain? | 59 | 90.77 | 44 | 70.97 | 0 | 0.00 | 8 | 12.90 | 6 | 9.23 | 10 | 16.13 | 11.120 | 0.004 | |||||||||||
| Periodontitis leading to an increase in serum TNF-α, CRP, IL-1, and IL-6 may induce insulin resistance by interfering with glucose and lipid metabolism. | 45 | 69.23 | 33 | 53.23 | 3 | 4.62 | 4 | 6.45 | 17 | 26.15 | 25 | 40.32 | 3.444 | 0.179 | |||||||||||
| Periodontal therapy improves the metabolic control in diabetics through insulin resistance and lessening the peripheral TNF-α. | 45 | 69.23 | 27 | 43.55 | 4 | 6.15 | 6 | 9.68 | 16 | 24.62 | 29 | 46.77 | 8.589 | 0.014 | |||||||||||
| Do you include taking a history of current or past dental infections as part of the physician’s examination for diabetic patients? | 61 | 93.85 | 37 | 59.68 | 3 | 4.62 | 23 | 37.10 | 1 | 1.54 | 2 | 3.23 | 21.537 | <0.001* | |||||||||||
| Do you think it is important to assess diabetic patients regularly for periodontal diseases? | 64 | 98.46 | 48 | 77.42 | 1 | 1.54 | 11 | 17.74 | 0 | 0.00 | 3 | 4.84 | 13.556 | 0.001* | |||||||||||
| Do you agree that primary factor responsible for type 2 diabetes mellitus is Insulin resistance? | 52 | 80.00 | 45 | 72.58 | 7 | 10.77 | 9 | 14.52 | 6 | 9.23 | 8 | 12.90 | 0.971 | 0.615 | |||||||||||
| Do you think a physician should refer patients with diabetes to a dentist for a comprehensive periodontal examination? | 60 | 92.31 | 45 | 72.58 | 2 | 3.08 | 12 | 19.35 | 3 | 4.62 | 5 | 8.06 | 9.720 | 0.007 | |||||||||||
| Do you think treatment of chronic periodontitis with scaling root planing, surgery (if indicated), selected tooth extraction (of hopeless teeth), and systemic antibiotics resulted in decreased insulin demand? | 34 | 52.31 | 25 | 40.32 | 14 | 21.54 | 12 | 19.35 | 17 | 26.15 | 25 | 40.32 | 2.981 | 0.225 | |||||||||||
| Do you think diabetes induces periodontitis? | 58 | 89.23 | 41 | 66.13 | 6 | 9.23 | 10 | 16.13 | 1 | 1.54 | 11 | 17.74 | 12.188 | 0.002** | |||||||||||
| Do you think periodontitis induces insulin resistance and worsen glycemic control? | 36 | 55.38 | 27 | 43.55 | 11 | 16.92 | 7 | 11.29 | 18 | 27.69 | 28 | 45.16 | 4.280 | 0.117 | |||||||||||
| Do you think management of diabetes, currently considered as epidemic in Indian subcontinent, is a “shared responsibility” of both dental as well as medical health care providers? | 62 | 95.38 | 56 | 90.32 | 1 | 1.54 | 2 | 3.23 | 2 | 3.08 | 4 | 6.45 | 1.235 | 0.539 | |||||||||||
| Do you refer your diabetic patients for routine dental check-up (for medical check-up if you are dental surgeons)? | 57 | 87.69 | 28 | 45.16 | 6 | 9.23 | 29 | 46.77 | 2 | 3.08 | 5 | 8.06 | 26.238 | <0.001* | |||||||||||
| Do you refer your patients for dental/medical care only when they had dental/medical complaints? | 35 | 53.85 | 40 | 64.52 | 28 | 43.08 | 18 | 29.03 | 2 | 3.08 | 4 | 6.45 | 3.105 | 0.212 | |||||||||||
| Do you refer your patients for dental/medical care only on patient’s request? | 17 | 26.15 | 26 | 41.94 | 47 | 72.31 | 28 | 45.16 | 1 | 1.54 | 8 | 12.90 | 12.077 | 0.002 | |||||||||||
A total of 3048 (127 × 24) responses of all the 127 participants for a total of 24 questions were recorded and analyzed. Among 1560 (65 × 24) responses of 65 OHCPs, 1240 (79.49%) “Agree or Yes,” 151 (9.68%) “Disagree or No,” and 169 (10.83%) responded “Unaware or No Idea” regarding DPI. Among 1488 (24 × 62) responses of 62 NOHCPs, 973 (65.33%) “Agree or Yes;” 233 (15.66%) “Disagree or No;” and 282 (18.95%) responded “Unaware or No Idea” regarding DPI. The difference in all three responses among OHCPs and NOHCPs was highly significant (P < 0.001).
Proportion of health care professionals having knowledge regarding “improvement of the glycemic control in diabetics through improvement in insulin resistance and lessening peripheral TNF-alpha after periodontal therapy,” thus role of periodontal therapy in the management of DM was 69% among OHCPs and was significantly higher as compared to NOHCPs (43%). Further, the results of the present showed that about 10% of NOHCPs denied whereas, 47% were unaware of this DPI. However, proportion of unawareness among OHCPs was about 25% only. Percentage of health care professionals having understanding that “primary factor responsible for T2DM is insulin resistance” was comparable among both OHCPs as well as NOHCPs. Similarly, more than 90% of all health care professionals consider that management of DM is “shared responsibility” of both OHCPs and NOHCPs.
DISCUSSION
The importance of oral health, of which periodontal health is a key component, to general well-being has been well documented.[11] Periodontitis may be a source of systemic inflammation that impacts overall health. Henceforth, OHCPs as well as NOHCPs (physicians) must be well informed about periodontal disease and its bilateral associations with systemic conditions to ensure best practices in patient care. Previous studies have shown varying levels of awareness of interrelationship between oral and systemic health among NOHCPs,[12,14,23,24] with limited awareness in developing countries.[11,12,23]
From the present study, it may be inferenced that overall “understanding and awareness” of DPI is better significantly among the OHCPs as compared to NOHCPs. Ayanbadejo et al.[15] reported that the association of DM with periodontal disease was particularly limited among the NOHCPs.
Umeizudike et al.[11] in a study among the residents of internal medicine in Nigeria, observed that majority had inadequate awareness of DPI. They related their results to the limited exposure of medical residents participating in their study to dental education, particularly during training in medical school.[11]
Results of the present study revealed that the level of “knowledge” and “attitude” of OHCPs was significantly better than that of NOHCPs for DPI. The level of response for “practice” of DPI was less than 60% for both OHCPs and NOCHPs. In contrast, Vellayappan and Varghese[18] reported that 82% of the medical doctors were aware of the DPI, and 58% of the doctors had the “practice” of referring patients with the systemic disease to dentists. In another study, Opeodu et al.[16] revealed that for DM, rheumatic heart diseases, valvular heart disease, and HIV/AIDS, more than 50% of NOHCPs strongly agreed with the possible causal link between oral diseases and systemic condition of individual patient, and 10% of the respondents strongly disagreed any existence of any possible link between oral health and of the systemic diseases.
Awareness of “epidemiology of type 2 DM” among world and Indian population revealed a higher proportion for knowledge among NOHCPs as compared to OHCPs. However, the difference was non-significant. Almost all health care professionals were having knowledge about “impact of DM on oral cavity” and results revealed that proportion of NOCPs about the same was significantly lower as compared to OHCPs. Loe reported, “periodontitis is the sixth complication of DM.”[25] Only 37% of NOHCPs were aware of this information, as compared to about 82% OHCPs.
Awareness regarding the impact of periodontal disease on systemic health and glycemic control,[6,26] and plausible underlying molecular mechanism involving oxidative stress and inflammatory status,[27] and immune-inflammatory response of host resulting in increased TNF-alpha, CRP, IL-1, and IL-6 that may induce insulin resistance due to chronic periodontitis,[8] was significantly higher among OHCPs as compared to NOHCPs. However, proportion among health care professionals for their attitude to include comprehensive oral and periodontal examination and periodontal therapy that results in a reduction in insulin demand, as part of ICP for management of DM[4,5] was significantly higher in OHCPs as compared to NOHCPs.
In the present study response to the questions framed to understand the current practice among health care professionals revealed that majority of OHCPs (87.69%) routinely refer their patients for medical health checkup or for seeking advice from physicians while treating diabetic patients, in contrast to only 45% of NOHCPs refer their patients to seek advice from OCHPs. Further results revealed that 46% of NOHCPs disagree with this referral concept, in contrast to 9% of OHCPs. Umeizudike et al.[11] reported that majority of medical respondents had a positive attitude about referring their patients for regular dental checkups, which is in contrast to the findings of the present study.
The present study inferred that awareness of DPI, among NOHCPs, was limited as compared to OHCPs. Henceforth, an increase in awareness of periodontal diseases[12,28] and its link to systemic conditions like DM can be improved among NOCHPs through the inculcation of ICP approach at undergraduate and postgraduate levels for budding health care professionals and continuing medical or dental education (CMEs/CDEs) for the practitioners. Even OHCPs, who have been taught about DPI during their graduation, are deficit, although their percentage is for less. These important findings exposed a lack of analytical skill and laxity in attitude among OHCPs that is predominantly associated with the management of tooth or teeth instead of looking at the patient as a whole and part of the community.
Although challenging, yet improved ICP approach to manage diabetes and periodontitis has been advocated by professional and scientific organizations.[29,30] Based on the results of the current study, it can be suggested that physicians can be made more aware of DPI so that they may include OHCPs for team management of DM. Regular visits of diabetic patients referred by NOHCPs to OHCPs offer opportunities for prevention, early detection and treatment of oral and periodontal diseases, and further prevention of diabetic complications. Since diabetes and periodontitis are both common chronic diseases affecting adults, so it might be beneficial for all dental offices to monitor the blood glucose levels of patients considered to be at risk for diabetes.[31] OHCPs should also refer their patients to physicians who respond poorly to initial periodontal therapy or have advanced periodontitis without obvious signs of poor oral hygiene for diabetes screening.
Majority of the health-care professionals appreciated the questionnaire-study for an updation regarding DPI. They further suggested that society in overall should be updated from time to time regarding recent studies and current trends in ICP management of chronic diseases. They recognized the need to fill the gap in knowledge and to contribute for the promotion of oral and periodontal health among their patients by emphasizing on routine oral health checkup to their patients and vice-versa as an important step in the overall management of DM. Community-level awareness programs for the general population, as well as patient counseling at the individual level about DPI by any health care provider, are of paramount importance. More space needs to be allocated to DPI in the medical curriculum to improve physician’s ability to contribute to oral health, and stress may be given to integrated teaching of medical and dental sciences to produce professionals who can serve humanity in a better way.[12]
Although the current study was short term, low sample size and carried out in local area of Lucknow, India, nevertheless, this study may be considered as an important step toward the management of DM through ICP approach in India, and can provide a basis for carrying-out long term, large sample, and multi-centric study.
CONCLUSION
Within the limitations of the study following conclusions can be drawn. Almost 79% of OHCPs were aware of the DPI. About 9% of OHCPs did not agree with DPI and 11% of OHCPs were “unaware” about the DPI. Similarly, about 65% of NOHCPs were aware of the DPI. About 15% of NOHCPs did not agree with DPI and 19% of NOHCPs were “unaware” about the DPI. The limited awareness observed among health care professionals participating in the present study highlighted a gap of KAP for DPI, which was higher among NOHCPs as compared to OHCPs.
Declaration of patient consent
Patient’s consent not required as this was a survey based study on heath care providers and their identity was not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr Vivek Kumar Bains is the editor of this journal. He does not have any competing interest.
References
- The impact of diabetes on periodontal diseases. Periodontol 2000. 2000;82:214-24.
- [CrossRef] [PubMed] [Google Scholar]
- National Health Policy. 2017. Ministry of Health and Family Welfare, Government of India. Available from: http://www.cdsco.nic.in/writereaddata/national-health-policy.pdf [Last assessed on 2017 Dec 16]
- [Google Scholar]
- Understanding the inter-relationship between periodontitis and diabetes: Current evidence and clinical implications. Compend Contin Educ Dent. 2016;37:368-70.
- [Google Scholar]
- Diabetes mellitus: Promoting collaboration among health care professionals. J Dent Hyg. 2009;83(Suppl 1):S3-12.
- [Google Scholar]
- Interprofessional collaborative practice models in chronic disease management. Dent Clin North Am. 2016;60:789-809.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiological relationships between periodontitis and systemic disease: Recent concepts involving serum lipids. J Periodontol. 2000;71:1375-84.
- [CrossRef] [PubMed] [Google Scholar]
- National Oral Health Survey and Fluoride Mapping: Dental Council of India New Delhi: Dental Council of India; 2004. p. :13. Available from: http://www.iaphd.org/nationalsurvey/summary.pdf [Last accessed on 2017 Dec 16]
- [Google Scholar]
- Relationship between periodontal disease and diabetes mellitus: An Asian perspective. Periodontol 2000. 2011;56:258-68.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of periodontal treatment in patients with periodontitis and diabetes: Systematic review and meta-analysis. J Appl Oral Sci. 2020;28:e20190248.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors of periodontal disease: Review of the literature. Int J Dent. 2014;2014:182513.
- [CrossRef] [PubMed] [Google Scholar]
- Association between periodontal diseases and systemic illnesses: A survey among internal medicine residents in Nigeria. Saudi Dent J. 2016;28:24-30.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness regarding the systemic effects of periodontal diseases among medical interns in India. J Glob Infect Dis. 2011;3:123-7.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontitis and sub-fertility; opinions and practices of Nigerian specialists. West Afr J Med. 2013;32:267-71.
- [Google Scholar]
- Knowledge, attitude, and practice of medical doctors towards periodontal disease. J Indian Soc Periodontol. 2013;17:137-9.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness of the effect of periodontitis on glycemic control type 2 diabetics: A pilot study. New Niger J Clin Res. 2012;2:209-15.
- [Google Scholar]
- An assessment of medical doctors' perception of possible interrelationship between oral and general health. Eur J Gen Dent. 2014;3:120-4.
- [CrossRef] [Google Scholar]
- Extent of awareness regarding periodontal disease in diabetic patients among medical interns. Nitte Univ J Health Sci. 2015;5:17-21.
- [CrossRef] [Google Scholar]
- A survey on knowledge, attitude and practice among the doctors towards systemic health possibly influenced by periodontitis. Int J Appl Dent Sci. 2017;3:190-2.
- [Google Scholar]
- Diabetic patients; level of awareness about oral health knowledge, attitude and practices. Pak Oral Dent J. 2011;31:292-5.
- [Google Scholar]
- Type II diabetes and oral health: Perceptions among adults with diabetes and oral/health care providers in Ghana. Community Dent Health. 2014;31:158-62.
- [Google Scholar]
- Survey on awareness and knowledge about the effect of diabetes mellitus on systemic and oral health in patients visiting general medicine outpatient department in dental hospital. J Krishna Inst Med Sci Univ. 2015;4:100-6.
- [Google Scholar]
- Knowledge attitude and practice regarding diabetes mellitus among non-diabetic and diabetic study participants in Bangladesh. BMC Public Health. 2017;17:364.
- [CrossRef] [PubMed] [Google Scholar]
- Extent of awareness regarding systemic effects of periodontal disease among medical interns. Ann Pak Inst Med Sci. 2013;9:188-90.
- [Google Scholar]
- Association between periodontal diseases and systemic diseases. Braz Oral Res. 2008;22(Suppl 1):32-43.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993;16(Suppl 1):329-34.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of improved periodontal health on metabolic control in Type 2 diabetes mellitus. J Clin Periodontol. 2005;32:266-72.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative and inflammatory status in Type 2 diabetes patients with periodontitis. J Clin Periodontol. 2011;38:894-901.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of periodontal infection on systemic health In: Newman MG, Takei HH, Klokevold PR, Carranza FA, eds. Carranza's Clinical Periodontology: A South Asia Edition (11th ed). New Delhi: Elsevier; 2012. p. :417-20.
- [Google Scholar]
- Management of periodontal disease in patients with diabetes good clinical practice guidelines: A joint statement by Indian society of periodontology and research society for the study of diabetes in India. J Indian Soc Periodontol. 2020;24:498-524.
- [CrossRef] [Google Scholar]
- Diabetes and periodontal disease: An update for health care providers. Diabetes Spectr. 2011;24:195-8.
- [CrossRef] [Google Scholar]