Translate this page into:
Treatment modalities for management of skeletal and dental Class III malocclusion – A case series
*Corresponding author: Soumyashree Biswal, Department of Orthodontics and Dentofaical Orthopedics, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. drsoumyashree53@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Panda S, Remin NM, Biswal S, Tandon R. Treatment modalities for management of skeletal and dental Class III malocclusion – A case series. Asian J Oral Health Allied Sci. 2024;14:5. doi: 10.25259/AJOHAS_25_2023
Abstract
Class III malocclusion is a challenging phenomenon to comprehend. Research done to determine the cause of Class III malocclusion revealed that the deformity affects all aspects of the craniofacial system, not only the jaws. Skeletal and dentoalveolar abnormalities coexist in the majority of patients with Class III malocclusion. Orthognathic surgery, dentoalveolar compensation, and growth modification are the three main therapies available for skeletal Class III malocclusion. Until the pubertal growth spurt, growth modification needs to be started. Thereby, in order to deal with skeletal Class III malocclusion in a grownup, orthognathic surgery collectively with conventional orthodontic therapy will be required in order optimize facial esthetics as well as attain stable occlusion. The objectives of the case series are to highlight different approaches to resolving skeletal Class III malocclusion, which includes orthognathic surgery, orthopedic appliance therapy, and extractions.
Keywords
Skeletal Class III
Extraction
Orthognathic surgery
Orthopedic
Class III molar relationship
INTRODUCTION
Class III malocclusions are one of the less common types of malocclusions that we see in everyday practice; yet, it is often more complicated to decide the treatment.[1,2] The etiology of Class III malocclusion can be multifactorial including genetic and environmental factors. It can occur either due to (1) retrognathic and/or small maxilla, (2) prognathic and/or large mandible, and (3) a combination of both.[3,4] The prevalence of the malocclusion in Indian population reported is about 3.4%.[5] There are many treatment modalities for the correction of Class III malocclusion ranging from growth modulation to surgical correction.[6] Non-surgical treatment modalities include the use of orthopedic appliances such as a face mask and chin cup for altering the growth of either maxilla or mandible or the use of camouflage for gaining arch alignment.[7] Surgical management includes mandibular setback or maxillary advancement along with presurgical orthodontics. This article presents three cases of Class III malocclusion treated in three different modalities.
CASE REPORT-1
A 22-year-male patient came to the department with the chief complaint of forwardly placed lower jaw. On clinical examination, it was revealed that the patient had a leptoprosopic facial form with a prominent chin, increased lower third of the face,and incompetent lips. Intraoral examination showed Angle’s Class III malocclusion, negative overjet of (–2) mm, and reverse overbite of 30%. The maxillary arch was constricted with anterior and posterior crossbite. Minimal crowding was present in the mandibular arch, with all permanent teeth present and good oral hygiene [Figure 1].

- Pre-treatment (a-c) extraoral and (d-h) intraoral photographs, (i) lateral cephalogram, (j) posteroanterior cephalogram, and (k) orthopantomogram.
Pre-treatment radiographic analysis
The lateral cephalogram of the patient indicated skeletal Class III with macrognathic and prognathic mandible and retrognathic maxilla and cervical vertebrae maturation indicator (CVMI) stage 6. The patient had a hyperdivergent growth pattern. Orthopantomogram showed a full complement of teeth. The posteroanterior cephalogram showed no gross asymmetry [Table 1].
| Skeletal Variable: | Mean | Pre-Treatment | Post-Treatment |
|---|---|---|---|
| SNA Angle (∘) | 820 | 790 | 830 |
| SNB Angle (∘) | 800 | 81 | 800 |
| ANB Angle (∘) | 20 | -20 | 30 |
| Go-Gn to S-N Angle (∘) | 320 | 330 | 370 |
| Lower Ant. Facial Height (mm) | 68 mm | 71 mm | |
| Eff. Max. Length (mm) | 85 mm | 85 mm | |
| Eff. Mandibular Length (mm) | 118 mm | 116 mm | |
| Y- Axis Angle (∘) | 660 | 580 | 640 |
| Facial Axis Angle (∘) | 00 | 00 | -20 |
| Sum of Post. Angles | 3960+60 | 3980 | 3980 |
| Dental Variables | |||
| U1 to N-A Angle (∘) | 220 | 310 | 330 |
| U1 to N-A (mm) | 4 mm | 5 mm | 6 mm |
| L1 to N-B Angle (∘) | 250 | 270 | 300 |
| L1 to N-B (mm) | 4 mm | 7 mm | 9 mm |
| L1 to A-Pog Line (mm) | 1 to 2 mm | 8 mm | 4 mm |
| L1 to Mandibular Plane (∘) | 900 | 900 | 1020 |
| Soft Tissue | |||
| S Line to U1 (mm) | 3 mm ahead of S line | 0 mm | |
| S Line to L1 (mm) | 6 mm ahead of S line | 3 mm |
SNA: Sella-Nasion-Point A, SNB: Sella-Nasion-Point B, ANB: Point A-Nasion-Point B, Go-Gn: Gonion-Gnathion, SN: Sella Nasion, Ant: Anterior, Eff: Effective, Post: Posterior, U1: Upper Incisor, L1: Lower Incisor, N-A: Nasion-Point A, N-B: Nasion: Point B, A-Pog: Point A Pogonion, S line: Soft tissue line
Diagnosis
Skeletal Class III base with Angle’s Class III malocclusion with Dewey’s modification type 3 in a non-growing patient with vertical growth pattern and incompetent lips.
Treatment plan
The treatment plan was ortho surgical. The decompensation of maxillary and mandibular arches was planned to be followed by bimaxillary surgery (LeFort I osteotomy for maxillary advancement and bilateral sagittal split osteotomy for mandibular setback).
Treatment progress
Pre-operative orthodontic preparation was conducted with a 0.022-inch slot McLaughlin, Bennett and Trevisi (MBT) prescription with posterior bite block. Leveling alignment started with 0.012 inch Nitinol arch wire and continued till 0.017 × 0.025 inch rectangular archwire [Figure 2]. Slight maxillary arch expansion was achieved by transpalatal arch appliance. Class II mechanics were used for retraction of maxillary incisors and proclination correction of mandibular incisors.
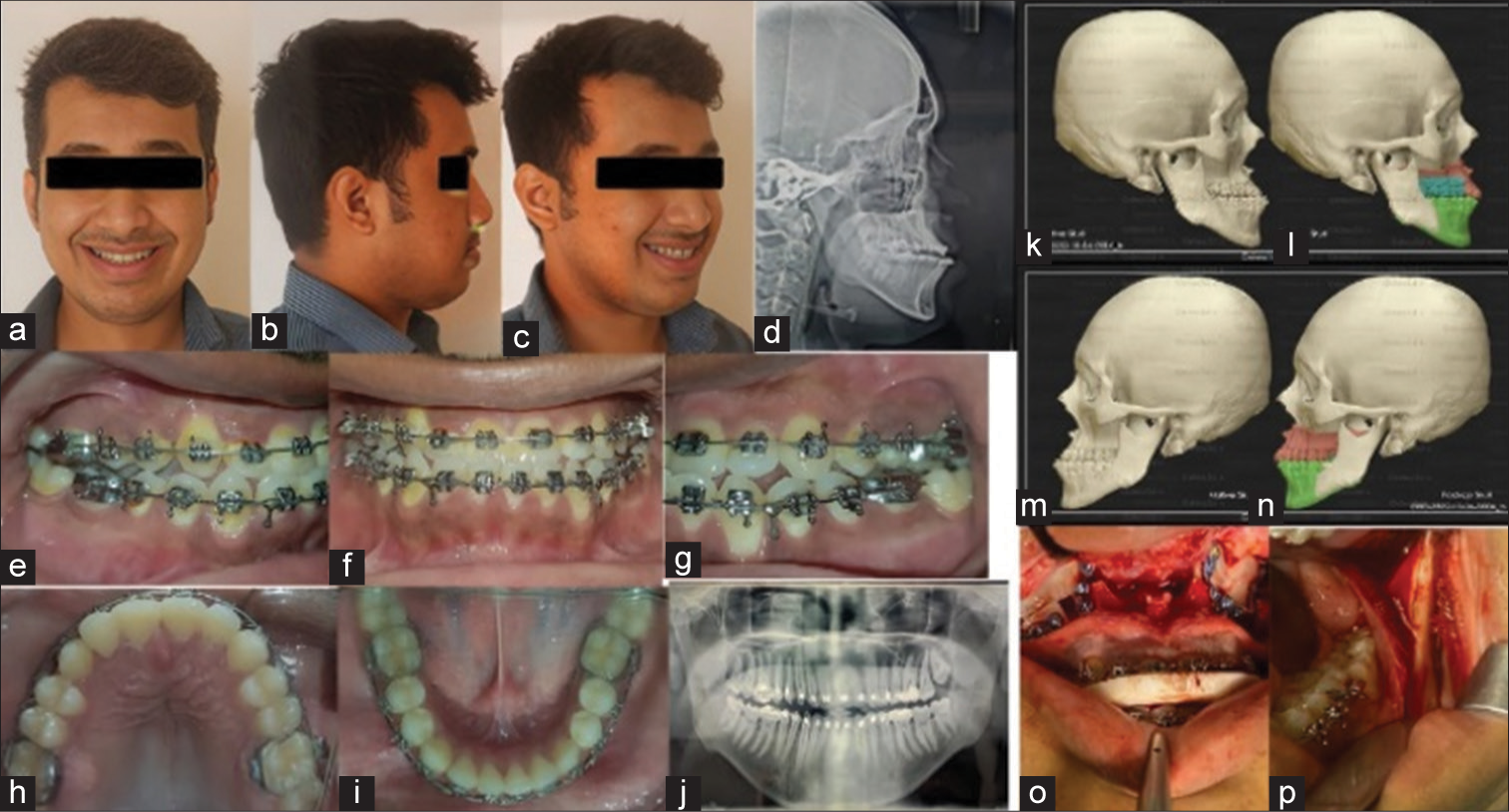
- Pre-treatment (a-c) extraoral, (d) lateral cephalogram, (e-i) intraoral photographs, (j) orthopantomogram, (k-n) three-dimensional surgical planning, and (o-p) intraoral photographs during surgery.
The surgical procedures included LeFort I osteotomy for advancement of the maxilla to correct the backward positioning of the maxillary arch. A total of 5 mm advancement of the maxillary arch was achieved. A bilateral sagittal split osteotomy was performed to achieve a mandibular setback by 4 mm. Rigid internal fixation was done using titanium plates and screws of 2 mm system.
Post-surgical management
Bimaxillary surgery (maxillary advancement 5 mm + mandibular setback 4 mm) was done. The patient was kept on Class III elastics to prevent any relapse postsurgically for six weeks. The surgical wires were removed and vertical settling elastics were given. A maxillary and mandibular fixed canine-to-canine retainer was placed [Figure 3].
- Post-treatment (a-c) extraoral and (d-h) intraoral photographs, (i) lateral cephalogram, (j) posteroanterior cephalogram, and (k) orthopantomogram.
Post-treatment assessment
The facial post-treatment photographs showed improvement in the facial profile. Ideal overjet and overbite had been achieved along with lip seal. The case was finished in Class I molar relation, Class I incisor, Class I canine, and premolar relation, and canine-guided occlusion.
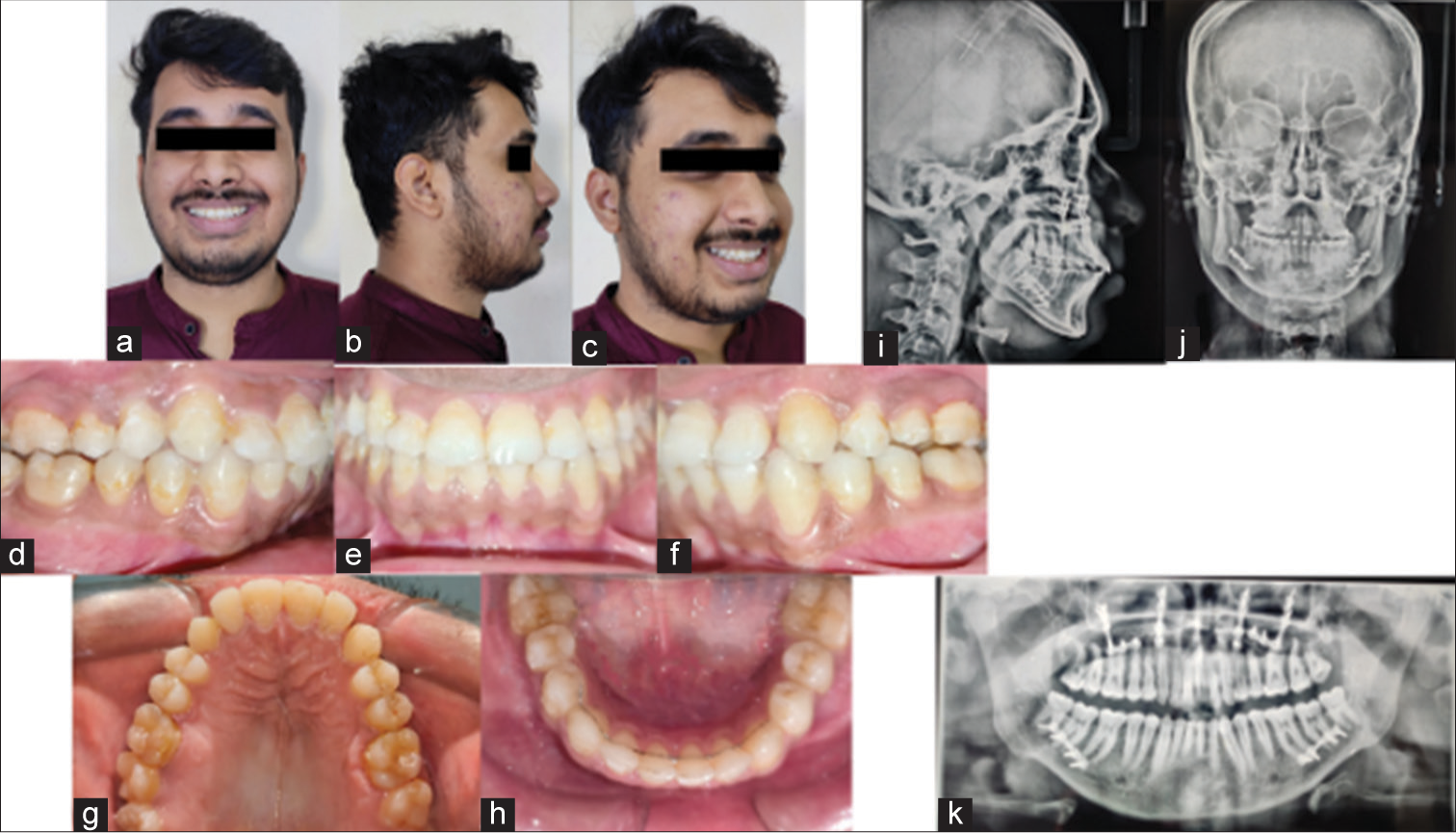
CASE REPORT-2
A 14-year-old female patient reported with a chief complaint of forwardly and irregularly placed lower front teeth. On clinical examination, the patient had a leptoprosopic facial form. There was no gross facial asymmetry detected. On intraoral examination, the patient has Class III molar and canine relation, end on anterior bite, overbite of 1 mm, and cross-bite wrt 12/43 and 22/33.
Pre-treatment radiographic analysis
Cephalometric findings [Table 2] showed a Class III jaw base with retrognathic maxilla and normal mandible with a vertical growth pattern. CVMI stage shows stage 3. Orthopantomogram (OPG) findings revealed missing 18.
| Skeletal Variable: | Mean | Pre-Treatment | Post-Treatment |
|---|---|---|---|
| SNA Angle (∘) | 820 | 800 | 790 |
| SNB Angle (∘) | 800 | 800 | 780 |
| ANB Angle (∘) | 20 | 00 | 10 |
| Go-Gn to S-N Angle (∘) | 320 | 420 | 410 |
| Lower Ant. Facial Height (mm) | 62 mm | 64 mm | |
| Eff. Max. Length (mm) | 75 mm | 78 mm | |
| Eff. Mandibular Length (mm) | 104 mm | 110 mm | |
| Y- Axis Angle (∘) | 660 | 620 | 640 |
| Facial Axis Angle (∘) | 00 | 40 | -30 |
| Sum of Post. Angles | 3960+60 | 4010 | 4010 |
| Dental Variables | |||
| U1 to N-A Angle (∘) | 220 | 290 | 220 |
| U1 to N-A (mm) | 4 mm | 6 mm | 6 mm |
| L1 to N-B Angle (∘) | 250 | 300 | 250 |
| L1 to N-B (mm) | 4 mm | 4 mm | 4 mm |
| L1 to A-Pog Line (mm) | 1 to 2 mm | 5 mm | 2 mm |
| IMPA (∘) | 900 | 880 | 870 |
| Soft Tissue | |||
| S Line to U1 (mm) | 0 mm ahead of S line | 0 mm | |
| S Line to L1 (mm) | 5 mm ahead of S line | 3 mm |
SNA: Sella-Nasion-Point A, SNB: Sella-Nasion-Point B, ANB: Point A-Nasion-Point B, Go Gn: Gonion-Gnathion, SN: Sella Nasion, Ant: Anterior, Eff: Effective, Post: Posterior, U1: Upper Incisor, L1: Lower Incisor, N-A: Nasion-Point A, N-B: Nasion: Point B, A-Pog: Point A-Pogonion, IMPA: Incisor Mandibular plane angle, S line: Soft tissue line.
Diagnosis
Skeletal Class III base with Angle’s Class III malocclusion with Dewey’s type 1 in a growing patient with vertical growth pattern with incompetent lips.
Treatment plan
Based on the clinical examination and cephalometric findings showing skeletal Class III due to maxillary deficiency and growth remaining, it was decided to treat the case with orthopedic appliance. It was planned to use a facemask for protracting the maxilla, along with maxillary arch expansion using bonded HYRAX. The timing of rapid maxillary expansion (RME) is critical because the start of fusion of the palatine portion of the suture could be imminent as the midpalatal sutures fuse between the ages of 15 and 19 years. Any correction later can be treated by surgically assisted RME because fusion of the mid-palatal suture already has occurred partially or totally, hampering the RME forces from opening the suture. The stage of ossification of MPS for the patient was stage c.[8] After achieving a normal skeletal relationship, the treatment with a fixed orthodontic appliance for finishing and detailing was planned in the second phase.
They were two stages of the treatment:
Phase 1
Orthopedic correction with facemask and RME.
Phase2
Dental correction and finishing and detailing.
Treatment progress
Phase 1
The patient was given an appliance which included a protraction facemask and bonded maxillary HYRAX screw. In the expansion, appliance hooks were placed on the buccal aspect near the permanent canines to engage the elastics for the facemask. The expansion appliance was cemented and an activation schedule of 90° turn two times per day was maintained for three weeks. The patient was advised to wear the appliance 12–14 h a day. The patient was advised to remove the appliance during eating and playing sports. Favorable improvements in the profile and radiographic changes were seen after the phase I therapy [Figure 4]. After the completion of the active phase, the chin cup was given for the retentive phase followed by fixed orthodontic treatment.
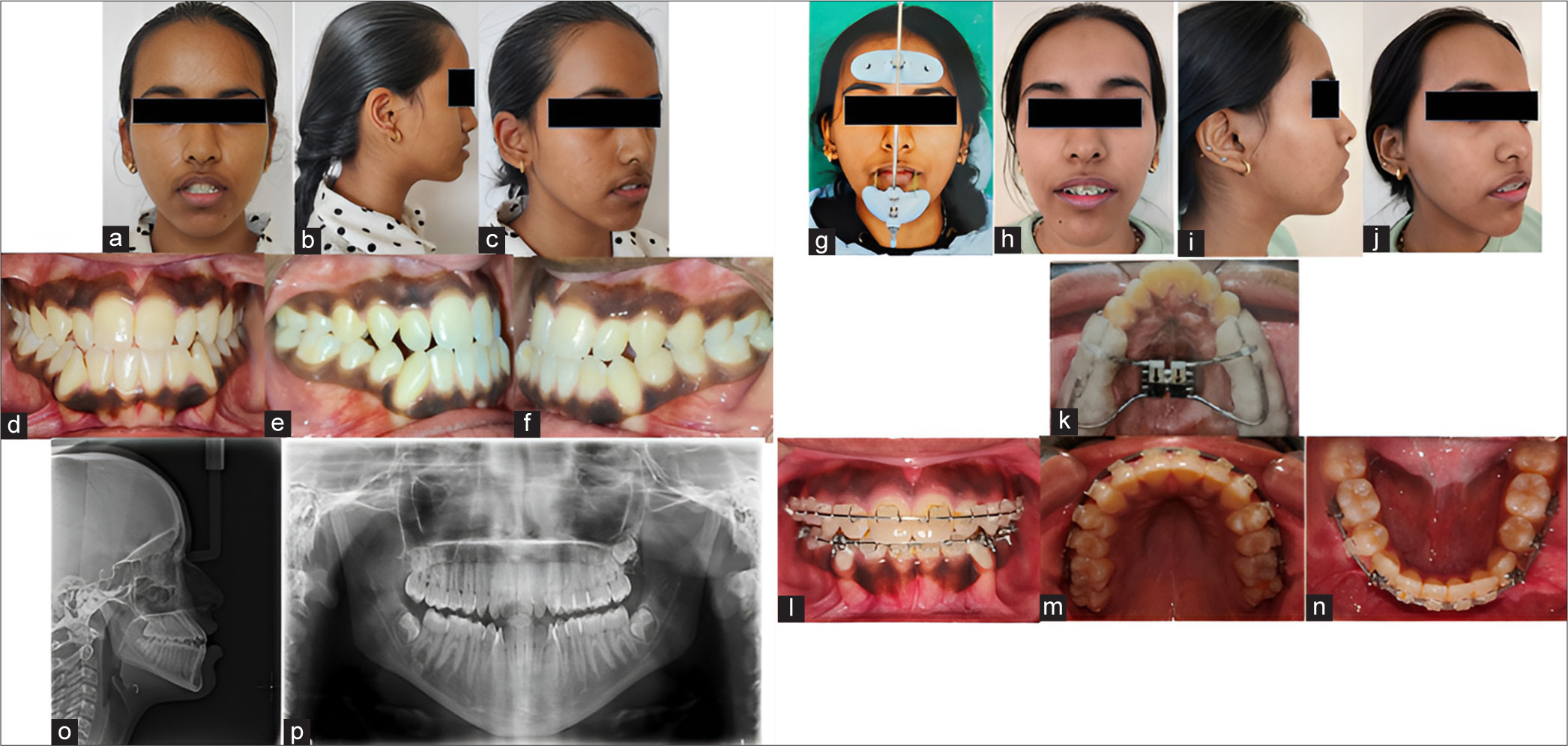
- Pre-treatment (a-c) extraoral and (d-f) intraoral photographs, stage treatment (g-j) extraoral and (k-n) intraoral photograph, (o) lateral cephalogram, and (p) orthopantomogram.
Phase II
Post orthopedic traction fixed orthodontic treatment was started with 0.022” slot MBT prescription. Extraction of the lower first premolars was done and initial leveling and aligning were done using Niti wires 0.014,” 0.018,” 0.016 × 0.022: followed by stainless steel wire 0.017 × 0.025. The hyrax screw was continued for the purpose of retention. The total duration of the treatment was about two years.
Treatment results
In the final stage of orthodontic treatment, improvement in facial profile was noted [Figure 5]. Well-aligned dental arches, normal overjet, overbite, and matching midlines were obtained.
- Post-treatment (a-e) extraoral and (f-j) intraoral photographs, (k) orthopantomogram, and (l) lateral cephalogram.
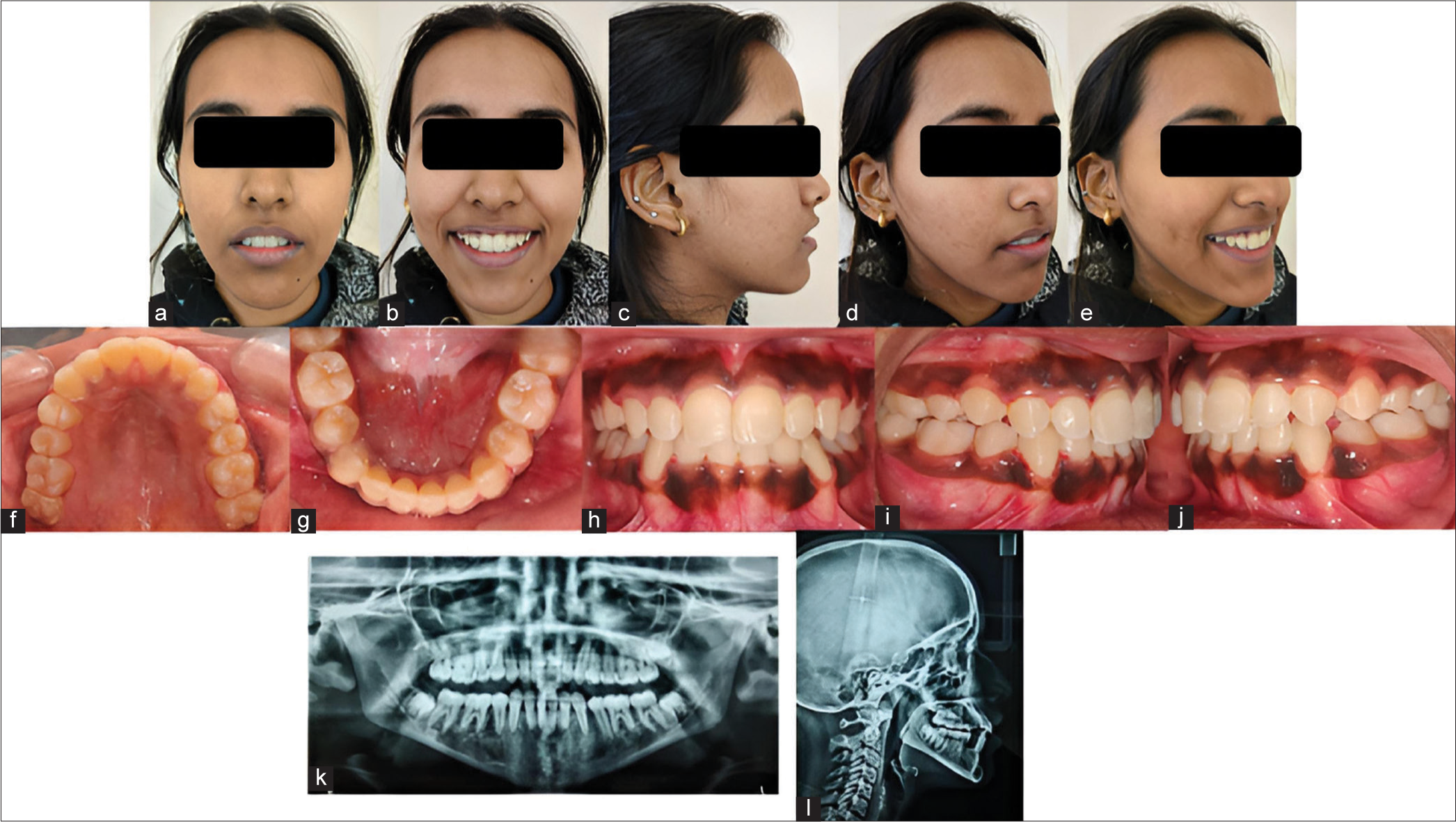
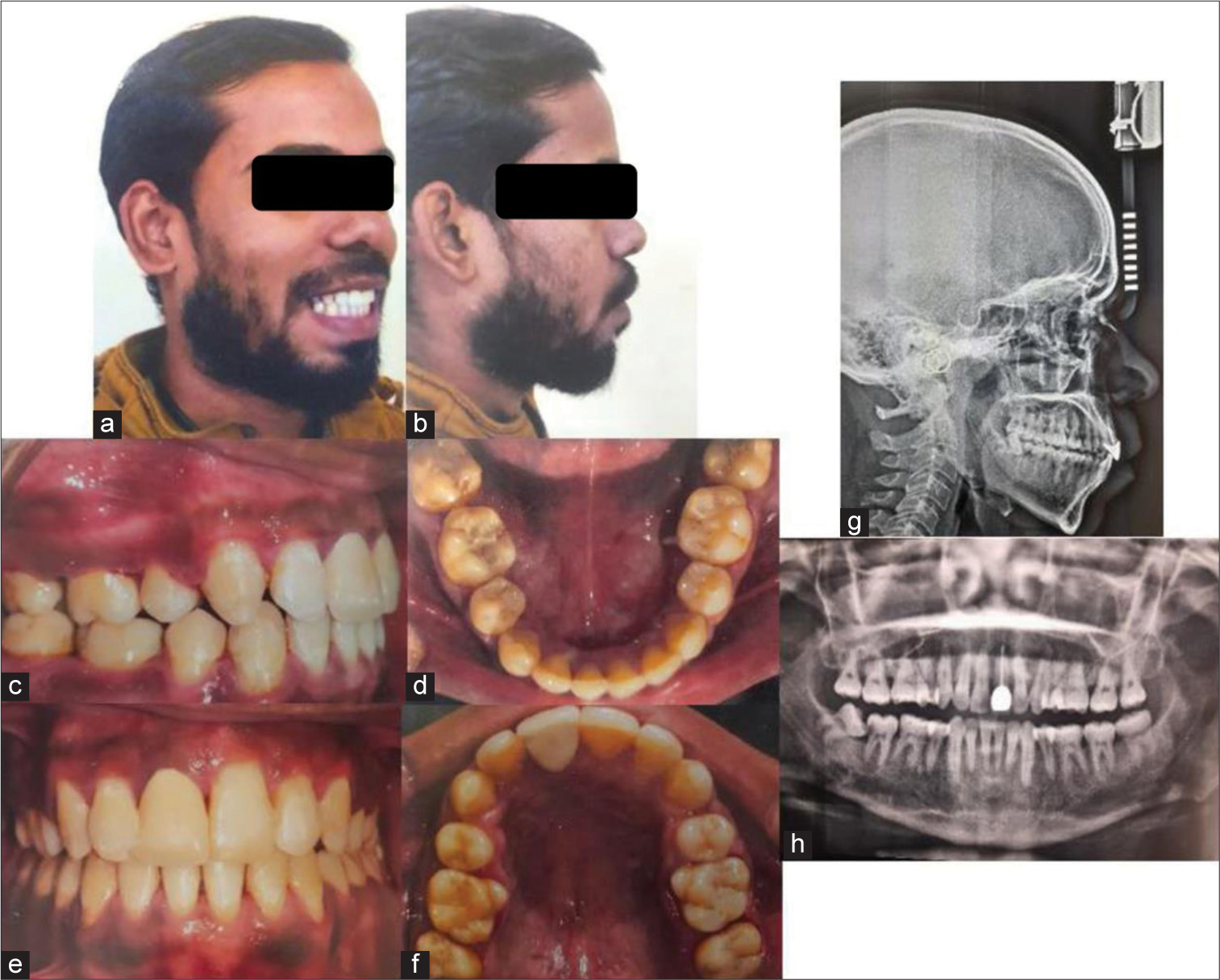
CASE REPORT-3
A 24-year-old male patient with history of Ellis and Davies Class IV fracture with respect to 11 teeth, nine years before, reported to the department with chief complaint of forwardly placed upper and lower teeth since past 6–7 years. His root canal treatment (RCT) wrt 11 tooth had been done five months back. On extra-oral examination, the patient had a convex facial profile with leptoprosopic facial form and straight facial divergence. The intraoral examination revealed that the patient had Angle’s Class III malocclusion with an edge-to-edge anterior bite and cross-bite with respect to 12/42 [Figure 6]

- Pre-treatment (a-b) extraoral and (c-e) intraoral photographs, (f) lateral cephalogram, and (g) orthopantomogram.
Pre-treatment radiographic assessment
The initial cephalometric analysis [Table 3] revealed that the patient had a skeletal Class II growth pattern with hyperdivergent growth pattern, prognathic maxilla and retrognathic mandible, and protrusive upper and lower lips and protrusive chin with CVMI Stage 6.
| Skeletal Variable | Mean | Pre-Treatment | Post-Treatment |
|---|---|---|---|
| SNA Angle (∘) | 820 | 850 | 840 |
| SNB Angle (∘) | 800 | 780 | 800 |
| ANB Angle (∘) | 20 | 70 | 40 |
| Go-Gn to S-N Angle (∘) | 320 | 390 | 370 |
| Lower Ant. Facial Height (mm) | 75mm | 72mm | |
| Eff. Max. Length (mm) | 84mm | 86mm | |
| Eff. Mandibular Length (mm) | 103mm | 103mm | |
| Y- Axis Angle (∘) | 660 | 660 | 650 |
| Facial Axis Angle (∘) | 00 | 20 | 20 |
| Sum of Post. Angles | 3960+60 | 4000 | 400 0 |
| Dental Variables | |||
| U1 to N-A Angle (∘) | 220 | 260 | 250 |
| U1 to N-A (mm) | 4 mm | 6mm | 5mm |
| U1 to S-N Angle (∘) | 1020 | 1100 | 1060 |
| L1 to N-B Angle (∘) | 250 | 440 | 410 |
| L1 to N-B (mm) | 4 mm | 44mm | 31mm |
| L1 to A-Pog Line (mm) | 1 to 2 mm | 16mm | 11mm |
| L1 to Mandibular Plane (∘) | 900 | 20 | 10 |
| Soft Tissue | |||
| S Line to U1 (mm) | 8mm | 5mm | |
| S Line to L1 (mm) | 11mm | 8mm |
SNA: Sella-Nasion-Point A, SNB: Sella-Nasion-Point B, ANB: Point A-Nasion-Point B, Go-Gn: Gonion-Gnathion, SN: Sella Nasion, Ant: Anterior, Eff: Effective, Post: Posterior, U1: Upper Incisor, L1: Lower Incisor, N-A: Nasion-Point A, N-B: Nasion: Point B, A-Pog: Point A-Pogonion, S line: Soft tissue line
Diagnosis
Skeletal Class II base with Angle’s Class III molar relationship and bimaxillary protrusion, Ellis and Davies Class IV fracture in respect to 11 teeth in a non-growing patient with hyperdivergent growth pattern and potentially competent lips.
Treatment plan
An extraction and retraction treatment plan was devised for this case. Full-mouth fixed appliance was bonded for leveling and alignment in the upper and lower dentition. Extraction of upper and lower first premolars was done to gain space.
Treatment progress
Orthodontic treatment was started with MBT 0.022” × 0.028” bracket system for initial leveling and aligning and arches were anchored with a transpalatal arch and lingual holding arch. Initially, treatment was started with 0.016” Ni-Ti round arch wire in maxilla and using 0.014” Ni-Ti round arch wire in the mandibular arch. The treatment continued till 0.017” × 0.025” rectangular archwire and Class III intermaxillary elastics were used to correct the molar relationship. Elastomeric chain and settling elastics were used for space consolidation and settlement of occlusion in the final stages of treatment. The treatment continued for 25 months and the treatment results were satisfactory [Figure 7]. The stability of the treatment outcome was ensured with Beggs wrap around retainer in the upper arch and fixed lingual retainer in the lower arch.
- Post-treatment (a-b) extraoral and (c-f) intraoral photographs, (g) lateral cephalogram, and (h) orthopantomogram.
DISCUSSION
Class III malocclusion is one of the most challenging cases to be treated successfully. The most common cause for this might be a combination of retrognathic maxilla and prognathic mandible. In such cases, the treatment plan might vary from non-surgical treatment options to surgical treatment plans. In our case series, various treatment modalities were used for treatment of Class III malocclusion where both surgical and non-surgical treatment plans were made, extraction along with chin cup therapy, extraction and expansion with facemask therapy, and surgical treatment where maxillary advancement and mandibular setback has been done. Fakharian et al, in 2019,[9] used mini-plate orthopedic treatment method as an alternative to surgery, which was effective in the elimination of the cross-bite and helping the patient achieve good facial esthetics. Haryani et al., in 2016,[10] described the management of a severe skeletal Class III malocclusion with bimaxillary orthognathic surgery in conjunction with fixed orthodontic appliance and extraction of upper first premolars.
CONCLUSION
This case series describes various treatment modalities in both growing and non-growing patients with skeletal Class III relationships which can be successfully obtained using different methods of treatment resulting in esthetically pleasing profile.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Biomechanics and esthetic strategies in clinical orthodontics Netherlands: Elsevier Health Sciences; 2005.
- [Google Scholar]
- Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56:7-30.
- [Google Scholar]
- Prevalence of malocclusion and its traits in Delhi children-I. J Indian Orthod Soc. 1995;26:98-103.
- [Google Scholar]
- Expanding limits for esthetic stratergies by skeletal anchorage In: Esthetics and biomechanics in orthodontics (2nd ed). Netherlands: Elsevier; 2015.
- [Google Scholar]
- Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am J Orthod Dentofacial Orthop. 2011;139:815-22.
- [CrossRef] [PubMed] [Google Scholar]
- Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofac Orthop. 2013;144:759-69.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal class III malocclusion treatment using mandibular and maxillary skeletal anchorage and intermaxillary elastics: A case report. Dental Press J Orthod. 2019;24:52-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of severe skeletal Class III malocclusion with bimaxillary orthognathic surgery. Contemp Clin Dent. 2016;7:574-8.
- [CrossRef] [PubMed] [Google Scholar]






