Translate this page into:
Advancement in periodontal accelerated osteogenic orthodontics: Exploring the synergy between periodontal and orthodontic treatment – A case report
*Corresponding author: Dhriti Gupta, Department of Periodontology, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. dhritigupta14@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta D, Singh A, Singh S, Jha AK, Chandra C. Advancement in periodontal accelerated osteogenic orthodontics: Exploring the synergy between periodontal and orthodontic treatment – A case report. Asian J Oral Health Allied Sci. 2024;14:16. doi: 10.25259/AJOHAS_12_2024
Abstract
Periodontally accelerated osteogenic orthodontics (PAOO) is a surgical technique that merges targeted corticotomy, particle grafting, and appropriate orthodontic forces. This approach shortens treatment duration, enhances tooth stability, and prevents the relapse of tooth movement. By leveraging the regional acceleratory phenomenon, PAOO promotes faster orthodontic tooth movement and improves the healing process of bone. It also increases the width of the alveolar bone, reduces the overall treatment time, enhances post-treatment stability, and minimizes the risk of dehiscence. The focus of this case study was to gauge the therapeutic effects of this surgical procedure alongside soft and hard-tissue augmentation in a patient undergoing treatment for orthodontic malocclusion.
Keywords
Corticotomy
Osteogenic
Periodontally accelerated osteogenic orthodontics
Bimaxillary protrusion
INTRODUCTION
Orthodontic treatment varies significantly across different age groups, with notable psychological, biological, and therapeutic differences. Individuals usually have distinct objectives to consider regarding cosmetic and dental esthetics. Along with the type of orthodontic appliances used, the duration of the treatment process is a major concerning factor for both, doctors and patients.[1] Misaligned teeth can adversely affect an individual’s quality of life by influencing functionality, physical appearance, and emotional well-being, often necessitating orthodontic intervention. This need for treatment is typically less pronounced in adults than in children, where growth changes are more evident. Furthermore, the cells of adults deploy and synthesize collagen fibers more gradually than in young adults. Finally, older individuals are more susceptible to periodontal challenges since their permanent teeth reside in the unmalleable alveolar bone.[2,3]
A number of individuals are uncertain about receiving conventional orthodontic therapy due to the duration of treatment. To address this concern, multidisciplinary dentistry is giving rise to new therapies involving periodontally accelerated osteogenic orthodontics (PAOO).[4] This treatment approach combines selective decortication-facilitated orthodontics with alveolar augmentation.[5] This approach can move a tooth rapidly in lesser time duration than conventional orthodontic therapy. Enhancing the efficiency of tooth movement has become a primary goal for clinicians, given the common adverse effects associated with prolonged orthodontic treatment, such as decalcification, root resorption, tooth mobility, periodontal issues, dental caries, loss of tooth vitality, temporomandibular joint disorders, and treatment relapse.[6]
PAOO treatment accelerates orthodontic tooth movement (OTM) by utilizing a regional acceleratory phenomenon (RAP), a bone healing pattern.[1,7] This treatment approach enhances alveolar bone width, alleviates the treatment period, augments post-treatment stability, and prevents dehiscence.[1,7,8]
Corticotomy-enhanced tooth movement was first time described by LC Bryan in 1893 and published in SH Guilford’s textbook. in 1993.[9,10] Kole’s paper in 1959 laid the groundwork for the development of the corticotomy-facilitated orthodontics.[11]
Kole gave an overview of the merged radicular corticotomy and supra-apical osteotomy procedure, which entails the reflection of full-thickness (mucoperiosteal) flaps by subjecting buccal as well as lingual alveolar bone, then executing interdental nicks across the cortical bone which hardly pierce the medullary bone.[11-13] Dibart later in 2009, reported a less invasive transmucosal corticotomy technique named as piezocision.[9]
Wilcko et al.[2] introduced an enhanced approach to advanced surgical orthodontic therapy. This combines corticotomy surgery and alveolar grafting in a technique referred as accelerated osteogenic orthodontics. Recently, this approach has transformed into PAOO.[14]
Studies have mentioned that this procedure is safe, effective, extremely predictable, related to less root resorption, shorter treatment duration, and may mitigate the need for orthognathic correction in certain cases.[15]
The key objective of this case report was to evaluate the clinical effects of PAOO combined with an allograft (Cologenesis Colocast Bone Graft) in a healthy adult with class I malocclusion, as well as a gingivoplasty of the palatal gingiva, with the objective to provide guidance regarding how to maintain the treatment’s effectiveness.
CASE REPORT
A 29-year-old female patient was referred to the periodontology department due to swelling around her upper front teeth, which had persisted for the past 2 months. She has no significant medical history, is not taking any prescription medications, and does not have any adverse habits.
The patient was unable to maintain proper oral hygiene due to fixed orthodontic treatment, which has been ongoing for the past year and a half. It was noted that the gaps between her teeth were taking longer to close than expected. She was undergoing fixed orthodontic therapy for class I malocclusion with bimaxillary protrusion and was referred to periodontology for PAOO to facilitate the closure of the spaces between the maxillary canines. The patient was selected for periodontal surgery after a thorough periodontal evaluation, which included case history collection with extra and intraoral examination to determine for facial abnormalities in the maxillofacial region.
The intraoral examination showed bilateral diffuse enlargement of the gingiva extending from the mesial of the right first premolar to the distal of the left first premolar in the maxillary arch. This enlargement involved the marginal, attached, and interdental palatal gingiva. The enlarged gingiva presented a reddish pink appearance causing minimal discomfort with loss of stippling (smooth and shiny) and rolled gingival margins. Subgingival calculus was present, along with slight bleeding upon probing. The enlargement was soft and edamatous, likely due to an inflammatory component related to poor oral hygiene during ongoing orthodontic treatment.
Based on the findings, the patient was advised to undergo initial therapy, hematological examination and surgical treatment. The treatment plan was laid down for the patient. Scaling and polishing were performed as part of the initial treatment. The patient was scheduled for a follow-up visit 3 weeks after phase 1 therapy. Hematological tests for hemoglobin level, bleeding time, clotting time, and random blood sugar were conducted, all of which fell within the normal range.
On the day of the surgery, the patient’s informed consent was obtained and vitals were recorded. This was followed by extraoral disinfection using 5% Povidone Iodine Solution, and intraoral disinfection was conducted with 10 mL of 0.2% Chlorhexidine, swished in the mouth for 1 min [Figure 1].

- Pre-operative (day 1).
Next, the surgical site was infiltrated with lidocaine 2% with 1:80,000 Adrenaline, administered buccally and palatally under all aseptic conditions. Gingivoplasty was performed using a scalpel on the palatal aspect.
A crevicular incision flap technique was used [Figure 2]. A full-thickness mucoperiosteal buccal flap was raised using a blunt periosteal elevator (P24G), and granulation tissue at the surgical site was thoroughly debrided [Figure 3].

- Crevicular incision on facial aspect.

- Elevation of full-thickness mucoperiosteal flap.
Vertical corticotomy slits were made on the alveolar bone between the roots from canine to canine on the buccal side of the maxillary arch at mesial and distal line angle of each root using a straight fissure bur in a contra-angle handpiece with abundant saline irrigation [Figure 4]. The vertical corticotomy slits were 1–1.5 mm deep onto the cortical bone [Figure 5]. An allograft (Cologenesis Colocast Bone Graft) mixed with saline was packed in the created vertical slits [Figure 6]. The flap was coaptated using interrupted sutures [Figure 7].

- Vertical slits prepared up to 1–1.5-mm depth at mesial and distal line angle of the root.
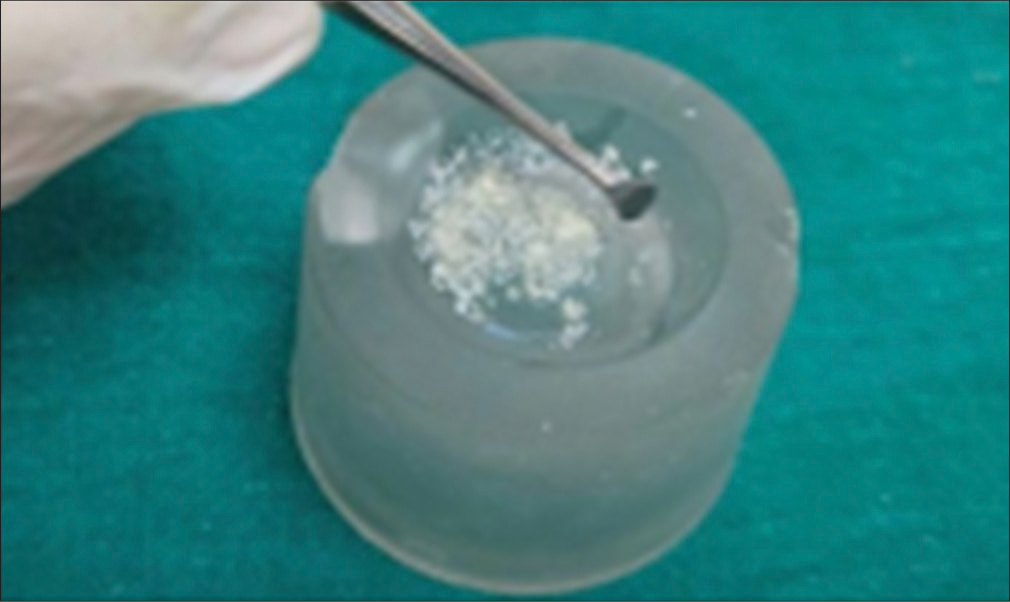
- Prepared bone graft (ColoGenesis Colocast bone graft).

- Placement of allograft (ColoGenesis Colocast bone graft).

- Approximation of flap and sutured.
The patient was briefed about post-operative instructions and dietary guidelines. Medications, Augmentin 625 mgTDS, Tramadol 50 mg-BD was prescribed for 5 days. The oral hygiene instructions given to the patient included advocating an alternative tooth brushing method (Charter’s toothbrushing technique) and the use of 10 mL of 0.2% chlorhexidine mouth rinse twice daily (not to spit forcefully) for 2 weeks post-surgery. Sutures were removed on the seventh day after surgical intervention. Uneventful and satisfactory wound healing was achieved at surgical site [Figure 8]. Patient was sent to department of Orthodontics and Dentofacial Orthopedics for further treatment, where complete space closure was achieved within 3 months.

- Follow-up after 3 months.
DISCUSSION
PAOO is a contemporary approach that employs selective alveolar corticotomy, particulate bone grafting, and orthodontic force to accelerate tooth movement.[16] The approach is gaining popularity because it can greatly reduce orthodontic treatment time while improving periodontal health and bone volume.[14,17]
PAOO has demonstrated a considerable reduction in treatment time, often by up to 50%, when compared with conventional orthodontics. In this case report, the patient’s treatment time was significantly decreased, resulting in optimal dental alignment.[18] This finding is consistent with previous research, which has shown that corticotomy induces a RAP that causes quicker tooth movement.[1,7] The RAP boosts bone turnover, allowing for faster tooth movement while yet providing periodontal support.[1,7] Additional bone grafting is required in PAOO to preserve alveolar bone volume, especially in cases where fast tooth movement may result in dehiscence or fenestration.[19]
Corticotomy-assisted orthodontics has been employed in many forms over the years to speed up orthodontic treatment. The initial hypothesis was that the cortical bone plates were the principal impediment to tooth movement and that by disrupting their continuity, the period of orthodontic therapy might be considerably decreased.[20] Although this procedure generated consistent results, pulp mortifications were not unusual.[21,22]
Following bone activation, particulate bone grafting is often conducted on the facial and palatal sides of the corticotomized sites.[22] Common grafting materials include deproteinized bovine bone, autogenous bone, decalcified freeze-dried bone allograft, or mixtures of these, which are compound grafts. While xenografts and synthetic materials can act as “osteoconductive” scaffolds for bone formation, they may not be adequate on their own.
Bone morphogenetic proteins contained in allografts may boost osteogenic capacity. Although data clearly support the significance of growth factors, it is suggested that volumetric expansion of the periosteum, which acts as a functional matrix for bone, plays an important role in producing the desired clinical outcomes.[23]
The quantity of graft material used is determined by parameters such as the projected direction and extent of tooth movement, the alveolar bone’s initial thickness, and the necessity for labial support from the alveolar bone. Typically, 0.25–0.5 mg of graft material is used per tooth.[11] Wilcko et al. proposed coupling demineralized freeze-dried bone and bovine bone graft with clindamycin. It is vital to avoid using a lot of graft material, as this can interfere with accurate flap placement. If there is a gingival recession, it can be corrected simultaneously with a connective tissue graft or an acellular dermal matrix allograft.[1,2]
According to Duker et al., aligning teeth following corticotomy can take 1½ to 3 months or less.[24] In a case of severe bimaxillary protrusion,[24] Chung et al. reported that full retraction of the anterior teeth combined with corticotomy was achieved in under 3½ months.[25] Germeç et al. revealed an enormous decrease in orthodontic intervention time, with a total duration of 16 months comparable to the overall treatment time of 31-month post-extraction procedures.[26]
Medications that limit bone turnover and increase calcium absorption may complicate these operations. Bisphosphonates and certain calcium compounds fall into this category.[27,28] Furthermore, osteopenia is a sterile inflammatory process that promotes tooth mobility, and certain other medications, particularly non-steroidal anti-inflammatory drugs, may decrease its effects. As a result, opioid analgesics are advised to manage post-operative pain.[29,30] Recent scientific investigation disclosed that prolonged transgenic overexpression of receptor activator of nuclear factor-kB ligand (RANKL) can expedite OTM that RANKL-specific gene recuperation can be utilized instead of corticotomy.
CONCLUSION
This case report demonstrates the effectiveness of PAOO in achieving accelerated orthodontic outcomes with minimal periodontal risk. The successful integration of corticotomy, bone grafting, and orthodontic force underscores the potential of this technique as a valuable tool in contemporary orthodontics. While the case adds to the growing evidence supporting PAOO, further studies are needed to explore its long-term stability and broader applicability across different patient populations.
Ethical approval
Ethical approval from Institutional Human Ethics Committee (IHEC) not required as patient anonymity is preserved and standard treatment protocols were provided.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21:9-19.
- [Google Scholar]
- Rapid orthodontic decrowding with alveolar augmentation: Case report. World J Orthod. 2003;4:197-505.
- [Google Scholar]
- Selective alveolar decortication for rapid surgical-orthodontic resolution of skeletal malocclusion treatment In: Bell WE, Guerrero C, eds. Distraction osteogenesis of the facial skeleton. Hamilton, BC: Decker; 2006. p. :199-203.
- [Google Scholar]
- The functional matrix hypothesis revisited. 1. The role of mechanotransduction. Am J Orthod Dentofacial Orthop. 1997;112:8-11.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontal accelerated osteogenic orthodontics: A description of the surgical technique. J Oral Maxillofac Surg. 2009;67:2160-6.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontal applications In: Atala A, Lanza RP, eds. Methods of tissue engineering. San Diego: Academic Press; 2002. p. :1207.
- [CrossRef] [Google Scholar]
- The innovated laser assisted flapless corticotomy to enhance orthodontic tooth movement. J Lasers Med Sci. 2012;3:20-5.
- [Google Scholar]
- Accelerated tooth movement by Corticision as an osseous orthodontic paradigm. Kinki Tokai Kyosei Shika Gakkai Gakujyutsu Taikai Sokai. 2006;48:6-15.
- [Google Scholar]
- Piezocision: A minimally invasive, periodontally accelerated orthodontic tooth movement procedure: Case report. Compend Contin Educ Dent. 2009;30:342-4, 346,348-50
- [Google Scholar]
- Orthodontia or malpositions of the human teeth: Its presentations and remedy Philadelphia, PA: T.C Davis and Sons; 1898.
- [Google Scholar]
- Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959a;12:277-88. contd
- [CrossRef] [PubMed] [Google Scholar]
- Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959b;12:413-20. concl
- [CrossRef] [PubMed] [Google Scholar]
- Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg Oral Med Oral Pathol. 1959c;12:515-29. concl
- [CrossRef] [PubMed] [Google Scholar]
- Accelerated osteogenic orthodontics-A case report. J Orthodon. 2012;39:122-128.
- [CrossRef] [PubMed] [Google Scholar]
- The regional acceleratory phenomenon: A review. Henry Ford Hosp Med J. 1983;31:3-9.
- [Google Scholar]
- Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontal. 1994;65:79-83.
- [CrossRef] [PubMed] [Google Scholar]
- An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: A synthesis of scientific perspectives. Semin Orthod. 2008;14:305-16.
- [CrossRef] [Google Scholar]
- The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res. 1989;248:283-93.
- [CrossRef] [Google Scholar]
- Periodontally accelerated osteogenic tooth movement in orthodontics: A review. Int J Adv Health Sci. 2015;1:32-7.
- [Google Scholar]
- Periodontally accelerated osteogenic orthodontics: A review of the literature. Balikesir Health Sci J. 2013;2:55-61.
- [CrossRef] [Google Scholar]
- Effects on the periodontium following corticotomy-facilitated orthodontics. Case reports. J Periodontol. 1990;61:234-8.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontally accelerated osteogenic orthodontics combined with autogenous bone grafting. Compend Contin Educ Dent. 2008;29:200-6.
- [Google Scholar]
- Experimental animal research into segmental alveolar movement after corticotomy. J Maxillofac Surg. 1975;3:81-4.
- [CrossRef] [PubMed] [Google Scholar]
- Lower incisor retraction with a modified corticotomy. Angle Orthod. 2006;76:882-90.
- [Google Scholar]
- Corticotomy facilitated orthodontics: Review of a technique. Saudi Dent J. 2010;22:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Accelerating tooth movement: The case against corticotomy-induced orthodontics. Am J Orthod Dentofacial Orthop. 2013;144:5-13.
- [CrossRef] [PubMed] [Google Scholar]
- The duration of orthodontic treatment with and without extractions: A pilot study of five selected practices. Am J Orthod Dentofacial Orthop. 1990;97:45-51.
- [CrossRef] [PubMed] [Google Scholar]
- The use of gene therapy vs. Corticotomy surgery in accelerating orthodontic tooth movement. Orthod Craniofac Res. 2011;14:138-48.
- [CrossRef] [PubMed] [Google Scholar]






