Translate this page into:
Prosthetic treatment of velopharyngeal insufficiency patient: A case report
*Corresponding author: Nikhil Kumar Sharma, Department of Prosthodontics and Crown and Bridge, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. nickinlv.nan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma NK, Pradhan I, Gaur A, Chopra D, Yadav P. Prosthetic treatment of velopharyngeal insufficiency patient: A case report. Asian J Oral Health Allied Sci. 2024;14:7. doi: 10.25259/AJOHAS_30_2023
Abstract
When the velopharyngeal valve exhibits an inability to autonomously close due to either insufficient tissue (velopharyngeal insufficiency) or inadequate movement (velopharyngeal incompetence), it leads to velopharyngeal dysfunction. Indications of this dysfunction encompass nasal liquid regurgitation, excessive nasal speech, nasal escape, speech articulation issues, and compromised speech comprehensibility. Managing velopharyngeal insufficiency through prosthetic intervention necessitates a closely coordinated effort between an otolaryngologist and a speech pathologist. This collaborative approach aims to facilitate socially acceptable speech patterns, prevent liquid seepage, and contribute to the rehabilitation of the patient.
Keywords
Velopharyngeal Insufficiency
Obturator Hypernasality
Fricatives
Syllables
INTRODUCTION
Clinicians face challenges in restoring velopharyngeal function for satisfactory speech using maxillofacial prosthetics. When the soft palate is partially or completely absent, leading to insufficient structure or altered function hindering closure with the pharynx, a pharyngeal obturator prosthesis becomes necessary.[1] This prosthesis aims to bridge the gap between the remaining hard and soft palates and the pharynx.
This case report outlines the clinical and laboratory procedures involved in crafting velopharyngeal obturator prosthesis for soft palate insufficiency. The goal is to mitigate nasal leakage of food and liquids and enhance speech integrity.
CASE REPORT
A 42-year-old man was referred from the Department of Plastic Surgery to the Department of Prosthodontics for the construction of a prosthesis to address a soft palate defect. The patient’s medical history revealed squamous cell carcinoma of the soft palate diagnosed in January 2021, which comes under group 1 defect of Vue’s classification [Figure 1]. He experienced liquid and food regurgitation through his nasal passage, significantly impacting both his personal and professional life due to hypernasal speech.

- Intraoral picture of the defect.
Examination
On examination, pronounced hypernasality and nasal escape were evident during assessments of nasal resonance by intermittently closing the nose while uttering/i-a/and/u-i/in the speech. Further, scrutiny revealed nasal escape during speech segments involving sustained fricatives such as/s/,/z/,/f/, and/v/. In addition, instances of substituting/b/with/m/and/d/with/n/were noted during the repetition of syllables/ba/,/bi/,/da/,/di/, in sentences, and in casual conversation.[1] Oral examination revealed the size and shape of a defect located in the posterior region of the palate [Figure 1]. During the speech, normal palatal mobility and elevation were observed.
Following evaluation, the defect was irrigated with normal saline and blocked with a wet gauge piece. With the help of a wooden stick, the defect was recorded with C-Silicone [Figure 2]. The primary reason for this step was to evaluate the accessibility of recording the defect in such a situation of restricted mouth opening. Next, the procedure for making the final impression was preceded by selecting the size of the perforated stock tray. Both, light body and C-Silicone impression material was loaded into the tray and placed in the patient’s mouth, and then the patient was asked to move his head in a circular manner, and to swallow and speak while the final impression was made [Figure 3]. The master cast was poured with dental stone. The maxillary record base was fabricated having retentive clasps made of 21 gauge stainless steel wire on premolar teeth.

- Impression of the defect.

- Secondary impression.
Wax-up was completed using modeling wax. Flasking and dewaxing were done, and the mold was packed with heat-cured clear resin and cured in two parts – first, the bulb portion and then the remaining part of the prosthesis.
The definitive position and contour of the obturator were determined with the prosthesis inserted into the mouth post-finishing and polishing and relined with a soft liner [Figure 4]. Pressure indicator paste identified areas of overextension. An oral examination was conducted with the prosthesis in place to assess the level of closure of the soft palate defect.
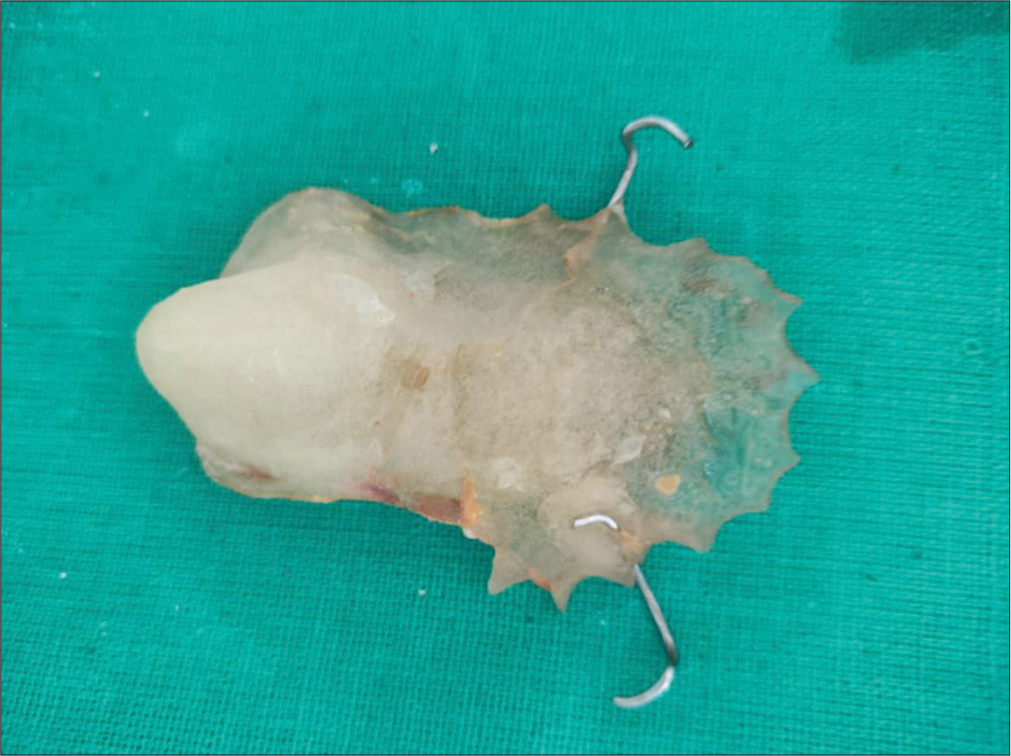
- Obturator.
Post-insertion instructions akin to those given to removable partial denture patients were provided to the patient.[2]
Post-prosthetic evaluation
The patient underwent speech assessments with and without the velopharyngeal prosthesis. Subsequent to the treatment, the patient was directed to a speech therapist for speech therapy and underwent a follow-up examination. The final evaluation post-prosthesis was conducted approximately three weeks after its fitting. Improvement in speech, particularly regarding hypernasality and comprehensibility, was observed both initially and throughout subsequent assessments.
Substantial improvements were noted in the management of nasal regurgitation of food and liquids.
DISCUSSION
This case report describes the fabrication and refinement of a hollow obturator prosthesis followed by speech therapy.
The velopharyngeal valve system regulates resonance, speech articulation, and various non-speech oral functions such as swallowing, blowing, sucking, and whistling.[3,4] Manifestations of velopharyngeal insufficiency encompass hypernasality, inappropriate nasal leakage, and reduced air pressure during the articulation of oral speech sounds, particularly weak pressure consonants.[5,6]
In instances where surgical intervention for velopharyngeal insufficiency is unsuitable due to localized or systemic reasons, patients become candidates for prosthetic treatment.[7-12] In the case of our patient, prosthetic intervention was specifically devised to effectively manage velopharyngeal insufficiency during wakefulness, addressing both speech and swallowing concerns.
CONCLUSION
Palatopharyngeal prostheses seem to be an effective treatment approach for patients suffering from palatopharyngeal insufficiency and cannot be treated surgically. The patient reported more acceptance of the prosthesis after the speech therapy sessions.
Reduced hypernasality, improved speech, and improved quality of life have been reported. The present report provides preliminary evidence that an intensive speech therapy program may enhance the effect of a speech bulb to reduce hypernasality in individuals with velopharyngeal dysfunction.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prosthetic management of velopharyngeal insufficiency induced by uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1995;113:611-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical management of the soft palate defect In: Taylor TD, ed. Clinical maxillofacial prosthetics. Germany: Quintessence Publishing Co. Inc.; 2000. p. :121-31.
- [Google Scholar]
- Maxillofacial rehabilitation In: Prosthodontic and surgical considerations. St Louis: Ishiyaku Euro-America; 1996. p. :285-329.
- [Google Scholar]
- Cleft palate and craniofacial anomalies: Effects on speech and resonance Clifton Park, NY: Cengage Learning; 2013.
- [Google Scholar]
- GOS.SP.ASS.’98: An assessment for speech disorders associated with cleft palate and/or velopharyngeal dysfunction (revised) Int J Lang Commun Disord. 1999;34:17-33.
- [CrossRef] [PubMed] [Google Scholar]
- Speech-aid prostheses for neurogenic velopharyngeal incompetence. J Prosthet Dent. 2000;83:99-106.
- [CrossRef] [PubMed] [Google Scholar]
- Therapy techniques for cleft palate speech and related disorders California: California Singular Publishing Group Inc.; 2001.
- [Google Scholar]
- Effect of a palatal lift prosthesis in individuals with velopharyngeal incompetence. Int J Prosthodont. 2009;22:579-85.
- [Google Scholar]
- Summer school speech therapy for children with cleft palate and language disorder. Gac Med Mex. 2009;145:475-9.
- [Google Scholar]
- The complementary use of speech prosthesis and pharyngeal flaps in palatal insufficiency. Cleft Palate J. 1964;1:194-8.
- [Google Scholar]
- Successful and rapid response of speech bulb reduction program combined with speech therapy in velopharyngeal dysfunction: A case report. Maxillofac Plast Reconstr Surg. 2015;37:22.
- [CrossRef] [PubMed] [Google Scholar]






