Translate this page into:
Prosthetic rehabilitation of a patient with ocular defect: A case report
*Corresponding author: Liyingbeni Lotha, Department of Prosthodontics, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. liyingbenil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Lotha L, Sharma NK, Chopra D, Gupta A. Prosthetic rehabilitation of a patient with ocular defect: A case report. Asian J Oral Health Allied Sci. 2024;14:13. doi: 10.25259/AJOHAS_7_2024
Abstract
Eye loss can lead to significant physical and psychological distress due to facial deformity. Rehabilitation options currently revolve around ocular prostheses, where resin has proven to be an effective material choice. Our clinical report explores a semi-customized approach, combining a stock iris with a customized sclera, which balances the advantages and disadvantages of both standard and custom prostheses. This solution aims to provide both esthetic appeal and functional effectiveness for individuals adjusting to the loss of an eye.
Keywords
Ocular defect
Rehabilitation
Prosthesis
Semi-customized
Stock iris
INTRODUCTION
The loss of a facial feature, particularly the eye, can result in serious psychological and physical issues. Cancers, congenital defects, irreversible trauma, excruciating blindness, and sympathetic ophthalmia are among the possible causes of eye loss.[1] Depending on the degree of involvement, three methods of surgery may be employed: Enucleation, exenteration, or evisceration.[2]
An ocular prosthesis that mimics the natural eye can significantly reduce the psychological distress associated with eye loss. The Egypt dynasty provided the first proof of replacing a missing eye using precious stones, earthenware, copper, and gold. Throughout the 19th century, materials such as celluloid and vulcanite were employed. Sand with little iron oxide was used by the Muller-Uri family to create glass eyes at the beginning of the 20th century. Various US military personnel worked together to successfully build the ocular prosthesis in 1944 using methyl-methacrylate resin.[3] Since then, resin use has become more common as a result of its benefits over alternative materials, which include its lightweight, translucency, enhanced fracture resistance, ease of manufacturing, ease of adjustment, and capacity for internal as well as external coloring.[4]
The literature describes various methods for creating and fitting artificial eyes. It comprises fitting a stock eye, creating a custom eye prosthesis, and modifying a stock eye on a positive duplicate of the ocular defect. The first two approaches are usually less time-consuming, but they often have disadvantages such as inconsistent fit and reduced esthetics. Custom ocular prostheses offer better fit and esthetics, but they are typically more difficult and time-consuming to make.[3-7]
This clinical report presents a method for creating an ocular prosthesis that is both aesthetically pleasing and functionally sound using a stock iris and custom-made sclera.
CASE REPORT
A 21-year-old male patient reported to the Department of Prosthodontics, Saraswati Dental College and Hospital, Lucknow, UP, India, with a chief complaint of facial disfigurement due to a missing right eye. The history revealed that it was a congenitally missing eye [Figure 1]. On examination of the eye socket, synchronous movements were observed and the posterior wall of the anophthalmic socket was covered with a healthy conjunctiva that showed no signs of inflammation or infection.

- Pre-operative view showing ocular defect.
Aggarwal et al.’s treatment-based classification approach placed the patient in Class 4 phthisis bulbi, which is defined as severe enophthalmos with deformed sclera and loss of orbital fat.[7]
Before starting treatment, the process was explained to the patient, and was given a semi-customized eye prosthesis with a customized sclera and stock iris.
Using Allen and Webster’s technique, an impression of the anophthalmic socket was created.[5]
SELECTION OF TRAY AND IMPRESSION
This technique made use of an impression tray shaped like an ocular prosthesis. To obtain the impression of the socket, light body addition silicone material (Orikam Neopure) was used [Figure 2].
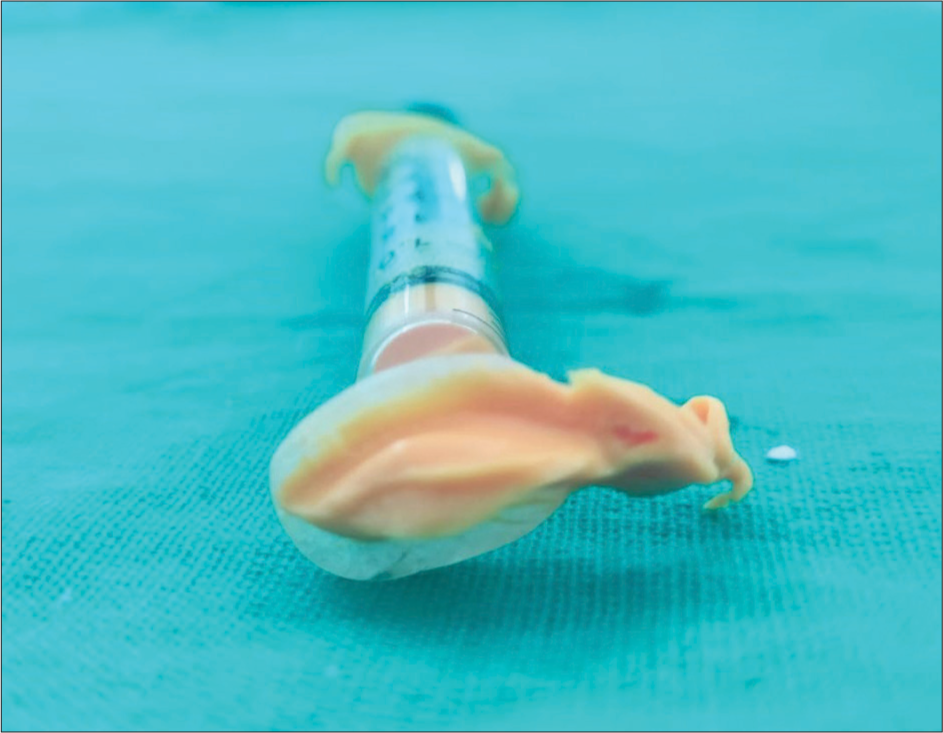
- Impression of the ocular defect made with light body addition silicone.
To take the impression, the patient is instructed to gaze straight ahead while the impression material is injected into the selected area using a syringe. The material is carefully filled into the defect, and the patient is asked to move their eye slowly in all directions. A small amount of material should flow out from the inner corner of the eye. The impression is then gently removed by first massaging the lower lid downward and away from the nose, followed by sliding the impression out from the upper eyelid in an arced path.
MAKING A STONE MODEL
The impression was filled with a dental stone (Kalabhai dental stone).
WAX CONFORMER OR SCLERAL TRYIN
Using a base plate wax (Modeling wax, Dental Products of India Ltd.), a wax conformer was made on the mold. After being removed from the mold, it was placed inside the eye cavity and examined for stability and esthetics. The anterior surface of the conformer received the required shape to resemble the features of the contralateral natural eye. A method as reported by Taicher et al. was used to enhance the conformer’s stability and esthetics even more.[6] After the wax conformer was reinserted into its socket, the patient was given instructions to move his head upright while moving the conformer and his natural eye in different directions. Due to this functional impression recording, the prosthetic eye can move in unison with the natural eye without coming loose from its socket. This modified wax conformer was employed in the creation of the acrylic resin eye prosthesis.
SELECTING AND POSITIONING IRIS
The contralateral natural eye was used as a guide to determine the iris’s size, color, and shape. From the stock eyes, the iris that matched the closest was chosen (American Optical Corp., Southbridge, Mass). A stock eye’s scleral portion was cut off with an acrylic trimmer. The scleral wax pattern was used to position the stock iris, and a hot tool was used to seal the border [Figure 3]. Using the graph grid method, the iris’ final position was determined in relation to the contralateral eye.[8] The natural eye was used as a guide when choosing the sclera’s shade.
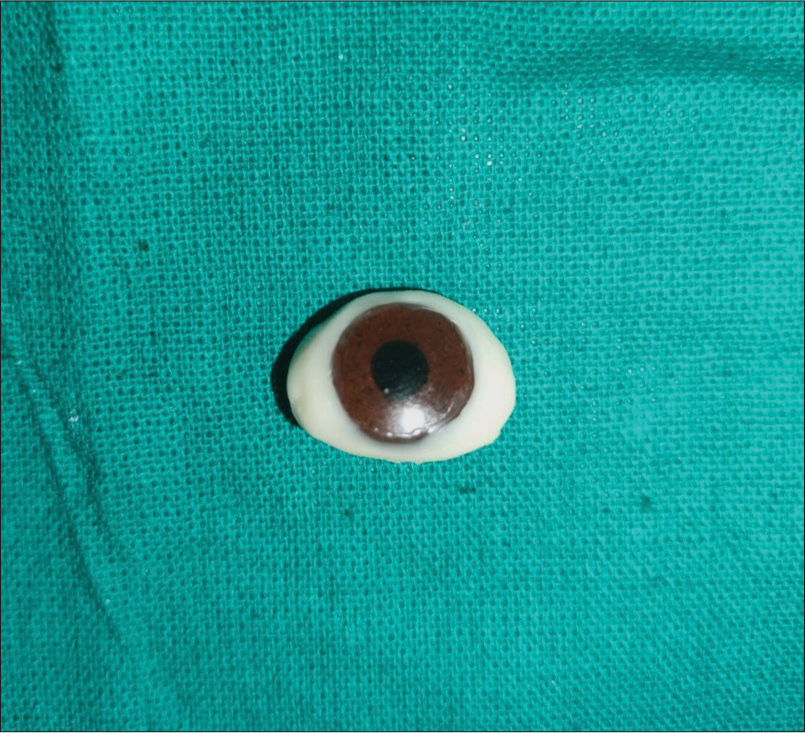
- Stock iris positioned on the scleral wax pattern.
FABRICATION OF RESIN SCLERA
After covering the scleral wax pattern with the stock iris, the pattern was removed from its socket. An autopolymerizing acrylic resin (DPI-Self cure, Dental Products of India, Ltd.) extension with a diameter of about 4 mm and a length of about 6 mm was affixed over the center of the stock iris in the mold to stabilize it. Conventional methods were used for flaking and dewaxing. A custom shade of heat-cure acrylic resin (DPI-Heat cure, Dental Products of India Ltd.) was poured into a pre-made mold [Figure 4].
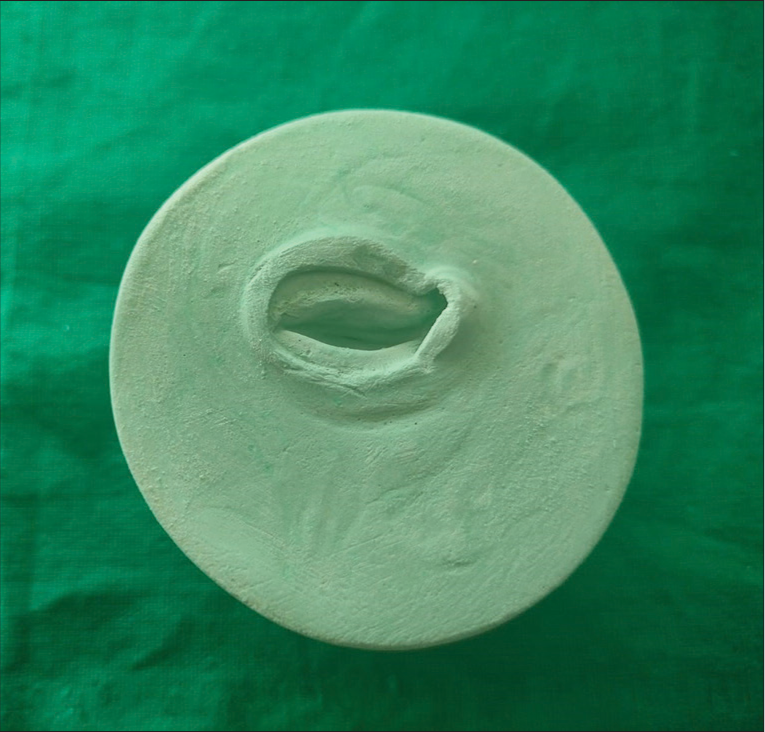
- Mold for acrylization.
After deflasking, the iris was attached over the resin sclera. After cutting the acrylic resin extension from the iris with an acrylic trimmer, polishing and finishing were done. The uncharacterized prosthesis was inserted into the socket. The iris’s position, the sclera’s shape, and the prosthesis’ stability were all reaffirmed.
FABRICATION OF THE FINAL PROSTHESIS
The prosthesis was finished, polished, deflasked, cured, and packed with clear heat-polymerizing acrylic resin to replace the trimmed sclera. After the final ocular prosthesis was placed into the socket, its fit, esthetics, and ability to move in unison with the opposing eye were assessed [Figure 5]. The patient received post-insertion instructions on how to use, take care of, and maintain the prosthesis.[9]

- Post-operative view showing the rehabilitation of the ocular defect.
DISCUSSION
The benefits of a customized ocular prosthesis over stock eyes are manifold, including enhanced contouring to fit the socket, precise color matching, and better synchronization of movements with the natural eye.[4,7,10] However, achieving these benefits requires the operator to invest additional time and expertise in customizing the iris.[11,12] This step becomes unnecessary if a stock iris that closely matches the patient’s natural eye on the opposite side is available. By adopting a semi-customized approach with a stock iris and a customized sclera, we can harness the strengths of both stock and custom prostheses. The prosthesis serves as a highly suitable esthetic and functional alternative for these patients. It aids in restoring patients’ self-confidence and prevents social awkwardness. It is important to note that this approach may not be suitable if there is a noticeable mismatch between the patient’s contralateral natural eye and the stock iris in terms of color, contour, or configuration.
CONCLUSION
The operator’s artistic abilities and the accuracy of the laboratory technique play a major role in the success of the ocular prosthesis. Due to the congenital absence of the eye, the rehabilitation of such cases presents challenges; nevertheless, extensive efforts have been made to address the issue effectively. With customized sclera, this procedure meets esthetic and functional criteria while requiring less artistic expertise and time due to the use of properly selected stock iris. A semi-customized ocular prosthesis can be used to conceal the operator’s diminished artistic ability. In patients who are indicated, this technique yields satisfactory results while cutting down on laboratory and clinical time.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Enucleation and evisceration In: Tasmun W, Jaeger E, eds. Duane’s clinical ophthalmology. Vol 5. Phildelphia, PA: Lippincott-Raven; 1995. p. :1-25.
- [Google Scholar]
- Surgical considerations in the prosthetic treatment of ocular and orbital defects. J Prosthet Dent. 1983;49:379-85.
- [CrossRef] [PubMed] [Google Scholar]
- The fitting and fabrication of a custom resin artificial eye. J Prosthet Dent. 1977;38:532-8.
- [CrossRef] [PubMed] [Google Scholar]
- Modified impression method of artificial eye fitting. Am J Ophthalmol. 1969;67:189-218.
- [CrossRef] [PubMed] [Google Scholar]
- Modified stock-eye ocular prosthesis. J Prosthet Dent. 1985;54:95-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prosthetic guidelines for ocular rehabilitation in patients with phthisis bulbi: A treatment-based classification system. J Prosthet Dent. 2014;111:525-8.
- [CrossRef] [PubMed] [Google Scholar]
- A simple method of positioning the iris disk on a custom-made ocular prosthesis. A clinical report. J Prosthodont. 2008;17:223-7.
- [CrossRef] [PubMed] [Google Scholar]
- Postinsertion care of the ocular prosthesis. J Prosthet Dent. 1983;49:220-4.
- [CrossRef] [PubMed] [Google Scholar]
- A simplified approach to rehabilitate an ocular defect: Ocular prosthesis. J Indian Prosthodont Soc. 2017;17:89-94.
- [CrossRef] [PubMed] [Google Scholar]
- Custom made ocular prostheses: A clinical report. J Prosthet Dent. 1996;75:1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Fabrication of ocular prosthesis step by step procedure: Case report. Int Dent J Stud Res. 2020;8:125-7.
- [CrossRef] [Google Scholar]






