Translate this page into:
Occurrence of internal root resorption defects in anterior teeth with a history of concussion injury: A cross-sectional study among select adult North Indian dental patients
*Corresponding author: Rhythm Bains, Department of Conservative Dentistry and Endodontics, King George’s Medical University, Lucknow, Uttar Pradesh, India. docrhythm77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bains R, Tikku AP, Verma P. Occurrence of internal root resorption defects in anterior teeth with a history of concussion injury: A cross-sectional study among select adult North Indian dental patients. Asian J Oral Health Allied Sci 2020;10:7.
Abstract
Objectives:
The aim of this study was to assess the frequency of internal resorption (IR) defects in select adult North Indian population with a history of concussion injury to their anterior teeth.
Material and Methods:
The study population consisted of patients reporting with a history of concussion injury to their anterior teeth. At least two intraoral periapical radiographs, one at central and other at a 20° horizontal angulation, were taken for each of the affected teeth to check for any IR defect. The radiographs were inspected after placing them over a viewing box using magnifying glasses. Percentage of IR defects and their occurrence on the basis of tooth type, duration of trauma, gender, and side was assessed.
Results:
A total of 1507 patients reported with a history of a traumatic dental injury (TDI) to their anterior teeth. About 37.1% (560/1507) patients and 602 teeth with TDI had a history concussion injury. The percentage of patients with concussion injuries resulting in IR defect was 3.3% (19/560), and the percentage of teeth with IR defect was 3.16% (19/602). About 68.42% (13/19) were in males, and 31.58% (6/19) were in females; however, the difference was not statistically significant (χ2 = 1.05, P = 0.590). Most of the patients reported with a history of TDI within 0–5 years back, and the median age at the time of presentation was 20 years. Maxillary left central incisor was most affected, 4.84% (9/186) followed by maxillary right central incisor 3.5% (7/200) mandibular left lateral incisor 3.85% (1/26), mandibular left central incisor 3.57% (1/28), and maxillary lateral incisor 1.52% (1/66). Out of the 19 IR defects, 15 (78.9%) were located in the root, four were located coronally (21.05%), out of which 2 had a pink-colored crown.
Conclusion:
Silent injuries such as concussion and subsequent IR can potentially weaken the tooth; therefore, follow-up of patients with a history of TDIs is vital to rule out any developing but obscure resorptive defects.
Keywords
Traumatic dental injury
Concussion
Internal resorption
INTRODUCTION
Even though the oral region comprises only 1% of the total body area, oral injuries account for up to 5% of all bodily injuries among all ages and about 17% in the age group of 0–6 years.[1] The teeth most commonly affected are the anterior teeth due to their position in the jaw, maxillary anterior being more vulnerable than the mandibular anterior.[2] The most frequent causes of traumatic dental injuries (TDIs) are alls, traffic accidents, fights, and sports.[3,4] Few cases of injury resulted from trauma to anterior teeth by sudden impact from hand pump handles have been reported from rural parts of India.[5] Increased overjet, inadequate lip coverage of the upper anterior teeth, predispose a person for these injuries.[6] Trauma to the tooth may lead to complete avulsion of the tooth, crown, or root fractures and luxation or concussion injuries, for which the patient seeks timely dental care.[7] However, sometimes there is no immediate fracture, and the tooth becomes asymptomatic after an initial phase of pain and tenderness to percussion, leading to the patient ignoring it and not reporting to the dental surgeon. These teeth, after an initial silent phase, may at a later stage become discolored, present with a sinus formation in relation to their root apex, and respond negatively to pulpal sensibility test.[8] According to Bakland and Andreason,[9] such injuries can be classified as concussion injuries and are defined as “An injury to the tooth-supporting structure without abnormal loosening or displacement of the tooth, but with increased reaction to percussion.”
One of the consequences of dental trauma is the resorption of dental hard tissue.[10] This may be external or internal, depending on the site of affliction, the former being more prevalent than the latter. Internal inflammatory root resorption is an invasive, inflammatory, resorption of the dental pulp, characterized by a widening or ballooning of the pulp space.[11] Although often termed idiopathic, the majority of the literature suggests trauma be the leading cause for IR of the tooth.[12] These defects, too, are generally asymptomatic and are accidentally diagnosed during a routine dental radiologic examination. Vital pulp tissue is a requisite for IR to occur and progress; however, by the time of its diagnosis, the pulp may have become necrotic. Timely detection and management of these lesions are critical, as if left unchecked, it may lead to extensive destruction and even perforation of the tooth surface.[13]
Epidemiological data on internal root resorption are scarce. As trauma to the tooth is cited as the leading cause of IR defect, this study was designed to assess IR defects in patients having a history of concussion injury to their anterior teeth as both concussion and IR are asymptomatic initially, but may be present silently.
MATERIAL AND METHODS
The study population consisted of patients presenting with discolored, traumatized, but intact anterior teeth, at the outdoor clinic of conservative dentistry and endodontics. Concussion injury was defined as a tooth with a history of trauma, but no signs of excessive mobility at the time of injury. At least two intraoral periapical radiographs, one at central and others at 200 horizontal mesial or distal angulation, were recorded on Kodak Ultraspeed films (Eastman Kodak Ultra-speed film; Kodak, Rochester, NY, USA) for each of the affected teeth to check for any IR defect and differentiate it from external resorption. The time elapsed between the incidence of trauma and dental examination was also recorded. Thermal tests using heated gutta-percha sticks and cold-pellets (Endo Frost, Roeko, Langenau, Germany) and electrical pulp sensibility tests (Digitest, Parkell Inc., Farmingdale, NY, USA) were performed to check the pulpal status. Teeth with discoloration without dental trauma or endodontically treated teeth, patients <18 years of age, and those with a history of complete avulsion of teeth or showing horizontal or vertical root fracture on IOPA were not included in the study. The radiographs were inspected by two endodontists after placing them over a viewing box using magnifying glasses. Any agreement between the observers was jointly re-evaluated until a consensus was reached. The criterion for IR defect was an oval-shaped radiolucency in the coronal or radicular pulp space, the position of which shifts along with the horizontal shift of the X-ray tube [Figure 1a and b].[14] The total percentage of an IR defect in anterior teeth and their occurrence on the basis of tooth type, duration of trauma, gender, and side were assessed. The data obtained were subjected to statistical analysis. The patients were informed of their condition, and after obtaining consent, the teeth with IR defects were treated according to the extent of the lesion and amount of remaining tooth structure.

- (a and b) IOPA radiographs showing internal resorption defect at two different angulations.
The results were analyzed using descriptive statistics and making comparisons among various groups. Data were summarized as proportions and percentages (%). All the associations were tested using the Chi-square test. Statistical analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). A P < 0.05 was considered statistically significant.
RESULTS
Out of 1507 patients with TDIs to anterior teeth, 37.1% (560/1507) patients and 602 teeth had a concussion injury. The percentage of IR defects in patients with concussion injuries was 3.3% (19/560), while the percentage of teeth with IR defect was 3.16% (19/602). The gender-wise analysis showed that 68.42% (13/19) IR defects were in males and 31.58% (6/19) in females; however, the difference was not statistically significant (χ2 = 1.05, P = 0.590). Out of the total teeth with IR defect, 12/19 were of the left side and 7/19 of the right side, but the difference was not statistically significant (P = 1.000). On inter arch comparison, 17/19 were seen in the maxillary arch and 2/19 in the mandibular arch [Table 1]. Among all teeth affected by trauma, maximum defects were recorded in the maxillary left central incisor 4.84% (9/186) followed by maxillary right central incisor 3.5% (7/200), mandibular left lateral incisor 3.85% (1/26), mandibular left central incisor 3.57% (1/28), and maxillary lateral incisor 1.52% (1/66). Fifteen (78.9%) of these were located in the root, four were located coronally (21.05%), and 2 of them had a pink-colored crown [Figure 2a and b]. According to the history of traumatic injury, 68.4% (13/19) patients had TDI 0–5 years back, 26.3% (5/19) patients >5, but <10 years back, and 5.3% (1/19) had TDI more than 10 years back. The median age for patients with a history of trauma in 0–5 years range was 20 years, and in patients with 5–10 age range which was 32 years [Table 2].
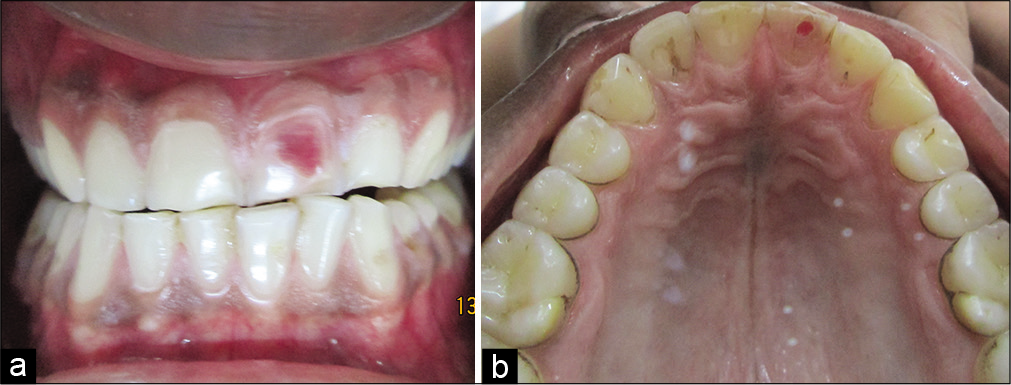
- (a) Pink tooth in relation to maxillary left central incisor (labial view). (b) Pink tooth in relation to maxillary left incisor (palatal view).
| Tooth number | Left side | Right side | P-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Maxillary lateral incisor (left side n=66 and right side n=68) | 1 | 1.52 | 0 | 0 | 0.492 |
| Maxillary central incisor (left side n=186 and right side n=200) | 9 | 4.84 | 7 | 3.5 | 0.686 |
| Mandibular lateral incisor (left side n=26 and right side n=4) | 1 | 3.85 | 0 | 0 | 1.000 |
| Mandibular central incisor (left side n=28 and right side n=24) | 1 | 3.57 | 0 | 0 | 1.000 |
Applied Fisher’s exact test for significance. Statistically, there was no significant difference observed according to side
DISCUSSION
The present study focused on patients with concussion injuries in the past, leading to tooth discoloration and eventual development of an IR defect. In the present study, 37.1% (560/1507) of the patients with TDIs showed the signs of concussion. In a survey evaluating the types of dental injuries and their pulpal sequelae among Nigerian adult patients, Oginni and Adekoya-Sofowora[15] reported concussion injury in 53% of the patients, while in children and deciduous dentition, the prevalence of 2.2% has been reported.[16] A more significant percentage of males 74.11% (415/ 560) experienced traumatic episodes compared to the females 25.89% (145/560), which is well in accordance with various past studies dealing with epidemiology of TDIs.[17] In the present study, maxillary central incisors were the most commonly affected, followed by the maxillary lateral incisors, with a slight predilection toward the left side. However, the difference was not statistically significant. Mandibular incisors were comparatively less affected, with the mandibular central incisors encountering more TDIs than mandibular laterals. The percentage of teeth negative pulp sensibility after a concussion injury was 32.5%, which is higher than 3% reported by Andearson and Pedersen[18] and 9.14% by Oginni and Adekoya-Sofowora.[15]
In the present study, the percentage of IR defects in teeth with concussion injury was 3.16% (19/602). Epidemiological data on the prevalence of IR are scarce, though some authors have reported a prevalence of 2.16% in anterior teeth of patients reporting to the endodontic clinic.[19,20] Haapasalo and Endal.[12] have suggested a prevalence of between 0.01% and 1% (patients affected) for internal inflammatory root resorption. Various other authors have recorded the development of defects in 28% of patients receiving vital pulp therapy,[21] and in 17% canines which were auto- replanted.[22] Maxillary central and lateral incisors were the most commonly affected teeth, which are in accordance with the available data on IR defects.[13] Most of the defects (15/19, 78.9%) had an intraradicular location. Males are reported to be more affected, as in the present study, also, the reason may be males encountering more traumatic injuries than females. However, the difference between the basis of side or gender was not significant. Most of the patients reported with a history of TDI within 0–5 years back, and the median age at the time of presentation was 20 years.
Concussion injuries are challenging to diagnose at the time of injury, as they are symptom-free initially, but may lead to eventual signs and symptoms of pulpal death. The guidelines by the American Association of Pediatric Dentistry on the management of acute dental trauma say that deciduous teeth have a high probability of maintaining a vital pulp after a concussion injury. In contrast, mature permanent teeth with closed apices may undergo pulpal necrosis due to associated injuries to the blood vessels at the apex and, therefore, must be followed carefully.[19] In the present study, patients with a concussion type of injury had not received any dental treatment with respect to the traumatized tooth until their time of reporting to the clinic. Few patients gave a history of having transient episodes of pain or pus discharge but had ignored them.
| History of trauma dental injury (years) | Male (n=13) | Female (n=6) | ||
|---|---|---|---|---|
| n | % | n | % | |
| 0–5 | 8 | 61.5 | 5 | 83.3 |
| >5 and ≤10 | 4 | 30.8 | 1 | 16.7 |
| >10 | 1 | 7.7 | 0 | 0 |
χ2=1.05, P=0.590; consider not significant
Internal inflammatory root resorption defect is clinically obscure, less prevalent, but one of the detrimental outcomes of TDIs. This process is brought about by the disruption of the external protective layer of predentin, thus exposing the underlying dentin to odontoclastic action.[19] Many times termed idiopathic; a majority of the patients give a history of trauma a long-time back. Factors that are said to trigger this clastic activity are trauma,[23,24] periodontal therapy, vital pulp therapy using calcium hydroxide,[21] or orthodontic treatment.[25] According to Haapasalo and Endal,[12] for the IR to start, vital pulp tissue should be present at the resorption area. In contrast, the pulp coronal to the resorption must be necrotic, allowing bacterial infection and microbial antigens to enter the root canal as the microbial stimulus is necessary for the continuation of IR.[12] It may be referred to as a silent killer, as it has no initial symptoms, and the clastic activity, if not diagnosed and managed timely, may keep progressing and weakening the tooth internally. Sometimes it may present as a “pink-tooth,” pertaining to an area on the crown of the tooth due to the hyperplastic, vascular pulp tissue filled in the resorbed area, showing through the thin overlying shell of the enamel.[10] Taking two IOPA radiographs using the Same Lingual Opposite Buccal or the cone shift rule are a safe, useful, and convenient aid in establishing the differential diagnosis from external resorption,[14] as the internal resorption defect will move with the tube-shift, while external resorption defect will not. Cone-beam computed tomography has proved to be an essential diagnostic tool as it gives a more accurate picture regarding the type, spatial configuration, and extent of the lesion. However, it may expose the patient to higher radiation dose compared to IOPA radiograph and should be performed in situations, where benefits outweigh the risks.[26]
CONCLUSION
Internal inflammatory root resorption can be potentially threatening to the integrity and longevity of the tooth structure; thus, efforts should be made to diagnose and manage it timely. Follow-up of the patients with a history of concussion injury, even with no apparent signs or symptoms, is important to rule out any developing but obscure resorptive defects. Epidemiologic data on resorptive defects are scarce. Thus, multi-centric studies with a larger sample size should be planned for a better understanding of this lesion.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Traumatic oral vs non-oral injuries. An epidemiological study during one year in a Swedish county. Swed Dent J. 1997;21:55-68.
- [Google Scholar]
- Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija. 2014;16:7-14.
- [Google Scholar]
- Incisortrauma in an adolescent Arab population. Prevalence, severityand occlusal risk factors. Am J Orthod Dentofac Orthop. 2005;128:347-52.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of traumatic crown fractures to permanent incisors in a childhood population: Móstoles, Spain. Dent Traumatol. 2003;19:119-22.
- [CrossRef] [PubMed] [Google Scholar]
- Splinting of longitudinal fracture: An innovative approach. Case Rep Dent. 2016;2016:5083874.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and associated factors of traumatic dental injuries in Brazilian school children. J Public Health Dent. 2010;70:313-8.
- [CrossRef] [PubMed] [Google Scholar]
- A proposal for classification of tooth fractures based on treatment need. J Oral Sci. 2010;52:517-29.
- [CrossRef] [PubMed] [Google Scholar]
- Response of oral tissue to trauma In: Andreasen JO, Andreasen FM, eds. Textbook and Color Atlas of Traumatic Injuries to the Teeth (3rd ed). Copenhagen: Munksgaard; 1993. p. :77-112.
- [Google Scholar]
- Dental traumatology: Essential diagnosis and treatment planning. Endod Topics. 2004;7:14-34.
- [CrossRef] [Google Scholar]
- Internal resorption: Clinical perspective and treatment challenges. Asian J Oral Health Allied Sci. 2015;5:37-43.
- [Google Scholar]
- Resorption: Part 1. Pathology, classification and aetiology. Br Dent J. 2013;214:439-51.
- [CrossRef] [PubMed] [Google Scholar]
- Internal inflammatory root resorption: The unknown resorption of the tooth. Endod Top. 2006;14:60-79.
- [CrossRef] [Google Scholar]
- Differential diagnosis of internal and external root resorption. J Endod. 1976;2:329-34.
- [CrossRef] [Google Scholar]
- Pulpal sequelae after trauma to anterior teeth among adult Nigerian dental patients. BMC Oral Health. 2007;7:11.
- [CrossRef] [PubMed] [Google Scholar]
- Study on prevalence of traumatic injuries in deciduous teeth of children aged from 6 to 60 months in the city of João Pessoa-Paraíba. RSBO. 2014;11:270-5.
- [Google Scholar]
- Epidemiology of traumatic dental injuries: A 12 year review of literature. Dent Traumatol. 2008;24:603-11.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis of luxated permanent teeth-development of pulp necrosis. Endod Dent Traumatol. 1985;1:207-20.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines on Management of Acute Dental Trauma. Am Acad Pediatr Dent. 2011;34:230-8.
- [Google Scholar]
- Study of prevalence of internal resorption in periapical radiography of anteriors permanents tooth. Int J Morphol. 2009;27:227-30.
- [CrossRef] [Google Scholar]
- Internal resorption of dentine; histopathologic control of eight cases after pulp amputation and capping with calcium hydroxide. Oral Surg Oral Med Oral Pathol. 1957;10:90-6.
- [CrossRef] [Google Scholar]
- Long term evaluation of autotrans planted maxillary canines with completed root formation. Acta Odontol Scand. 1983;41:23-31.
- [CrossRef] [PubMed] [Google Scholar]
- Root resorption following traumatic dental injuries. Proc Finn Dent Soc. 1992;88:95-114.
- [Google Scholar]
- Internal resorption complicating orthodontic tooth movement. Br J Orthod. 1983;11:155-7.
- [CrossRef] [PubMed] [Google Scholar]
- The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography: An in vivo investigation. Int Endod J. 2009;42:831-8.
- [CrossRef] [Google Scholar]






