Translate this page into:
Let’s review the intermaxillary elastics in orthodontics
*Corresponding author: Ghazia Tarannum, Department of Orthodontics and Dentofacial Orthopedics, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. ghaziarza00@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tarannum G, Shaw T, Tandon R. Let’s review the intermaxillary elastics in orthodontics. Asian J Oral Health Allied Sci. 2024;14:10. doi: 10.25259/AJOHAS_3_2024
Abstract
Elastics play an important role in orthodontic treatment by exerting forces on the teeth and jaws to achieve proper alignment and correct malalignment. These are commonly used in combination with braces and/or with other orthodontic appliances to help move the teeth into their desired positions. The use of elastics is believed to arise from many years ago for different purposes in orthodontics. Intraoral elastics can be classified into sagittal, transverse, and vertical planes, and according to force delivery, elastics can be high pull, medium pull, and heavy pull. Like every dental material, elastic also has some delusion, side effects, and force decay properties with respect to time. Clinically, it is important to have an appropriate knowledge of the desired positive effects and the possible adverse effects that are normally associated with the use of elastic mechanics by orthodontists.
Keywords
Elastics
Intraoral
Force decay
Orthodontics
Intermaxillary
INTRODUCTION
Orthodontics is a specialized branch of dentistry that focuses on the prevention, intervention, diagnosis, and treatment of dental and facial irregularities. One common tool used in orthodontics is intraoral elastics. Intraoral elastics, also known as rubber bands, are an integral part of orthodontic treatment. They are used to apply forces to the teeth and jaws, helping to correct misalignment and achieve proper alignment.[1] These elastics are typically made of latex or synthetic materials and are available in various sizes, colors, and strengths.[2] Originally, latex was the only material used to make the elastics, which are still the most popular today. Nonetheless, artificial orthodontic elastics are currently being manufactured, providing a choice for patients who experience latex allergies.[3-8]
The intraoral elastics in orthodontic treatment are used for achieving desired tooth movement and maintaining anchorage during treatment and they play a crucial role in orthodontic treatment by exerting forces on the teeth and jaws to correct malalignment.[9] Elastics are commonly used in conjunction with braces or other orthodontic appliances to help move the teeth into their desired positions.[10] They can be attached to brackets on the teeth or to hooks on orthodontic wires, depending on the specific treatment plan. These elastics work by applying a continuous force on the teeth, gently guiding them into the desired position.[11]
Using intraoral elastics as an alternative to surgery offers a non-invasive approach that many patients prefer. This can be particularly beneficial for those who are averse to surgical procedures. In addition to avoiding surgery, orthodontists may use alternative treatment modalities such as Class II elastics, extractions, extraoral traction, orthodontic distalizers, temporary anchorage devices (TADs), and fixed functional appliances to address malalignment and achieve the desired results.[12] Elastics have a number of drawbacks, including the need for patient cooperation, deterioration in the oral environment, and side effects such as occlusal plane asymmetries, root resorption, allergic reactions, and dental rotations.[4,13-23]
MATERIALS AND METHODS
An extensive search was done among the orthodontic literature with the use of PubMed, Google Scholar, and Research Gate using the keywords “Elastics AND orthodontics,” “Intraoral elastics OR Orthodontic elastics.” The included articles were those which reported different types of connections used for elastic placement and various types of intraoral elastics.
HISTORICAL PERSPECTIVE
The use of elastics is believed to have stemmed many years ago when the Mayans and Incans utilized natural rubber for different purposes. Natural rubber is considered the first-ever elastomer (rubbery material) that can return to its original shape even after extended periods of stretching. Charles Goodyear, an American engineer and chemist, created the vulcanization process. When the vulcanization process became more popular, more people and businesses started using natural rubber.[24] At the Columbia Dental Congress, Calvin Case talked about using intermaxillary elastics. Nonetheless, the use of intermaxillary elastics is credited to Henry A. Baker. The Baker anchorage was first used by Henry A. Baker in 1893. It involved using intermaxillary elastics with rubber bands.[25-27] Dr. Calvin Case, an orthodontist states that he was the first clinician to use intermaxillary elastics. However, the father of American orthodontics, Edward Angle, along with other colleagues, believed that it was Dr. Baker who pioneered elastics in orthodontics and not Dr. Case.[28,29] He presented the method to the New York Institute in 1902.
However, more importantly, there was a problem with natural rubber. Its elasticity decayed within a short span of time because when the elastics stay inside the oral environment, the rubber would begin imbibing water. As a result, the elastics deteriorated swiftly. It was later decided that latex elastics should replace natural rubber in the early 1900s. Around the 1960s, synthetic elastics were developed and soon became the choice material for orthodontics.[30,31]
ELASTIC BANDS
Elastic bands are manufactured by slicing rubber tubes of different lumen and wall thicknesses. The lumen of the band and its wall thickness determines the force value when stretched. Within each size of the lumen, there are three types of bands – light, medium and heavy; in terms of their force value [Figure 1]. According to lumen size – the lumen of the elastic band is usually expressed in parts of an inch. For example – a 3/8 inches rubber band means that the lumen of the band is three parts of the eight parts of an inch.
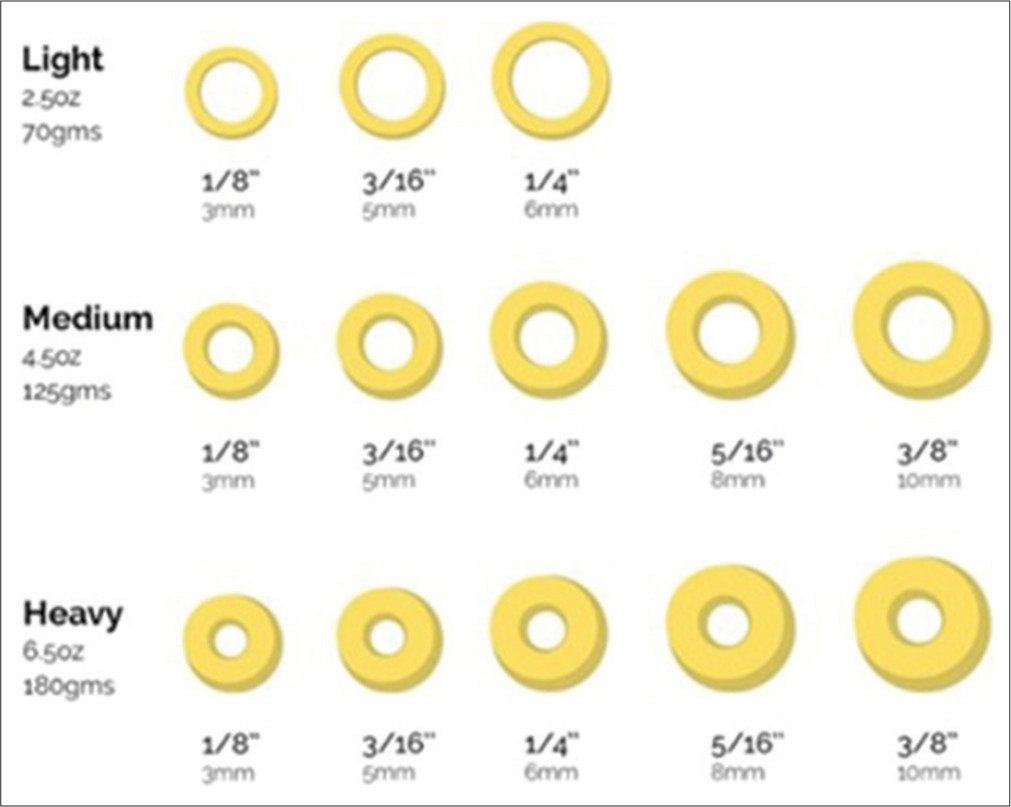
- Lumen sizes of elastics.
PRE-STRETCHING OF ELASTICS
Wong suggested in 1976 that the elastomeric materials be pre-stretched to 1/3rd of their length. This procedure will increase the length of a material. If the material is overstretched, a slow set will occur but will go back to the original state in time. If the material is overstretched to near breaking point, over and over again, permanent plastic deformation will occur. This means that the initial force may come to an effect during a pre-stretched process. Hence, when it is in use, it will give a more stable force. [25,32]
TYPES OF INTERMAXILLARY ELASTICS

- (a) Class II; (b) Class III; (c) anterior elastics; (d) cross elastics; (e) triangular type 2; (f) triangular type 3; (g) delta; (h) m elastics; (i) sling shot; (j) midline; (k) box elastics; and (l) intermaxillary elastics for aligners (modified from Farret, 2023).
| Anchorage | Connection | Size | Force | Wear time | |
|---|---|---|---|---|---|
| CLASS II | Rectangular stainless steel wires, preferably 0.019 × 0.025-in. Tip-back bends with step-down and accentuated toe-in on the lower second molar. In lower incisors, a buccal root torque. In the maxillary arch, the torque of the incisors must be increased. |
Ideally, from welded or clipped hooks in the region between the lateral incisor and canine (preferably placing downward/occlusally) to lower second molars. | 1/4-in, 5/16-in, or 3/8-in medium strength elastics. | 200 g each side | Active phase- 24 h each day. Post-retention phase- 12 h each day for a month. |
| CLASS III | Rectangular stainless steel wires, preferably 0.019 × 0.025-in. Tip-back with step-up and accentuated toe-in bending on the upper second molar. Lower incisors- a lingual torque. | From hooks welded in the region between lower lateral incisor and canine to maxillary second molars. | 1/4-in, 5/16-in, or 3/8-in medium force | 200 g each side | Same as in class II |
| Vertical elastics (intercuspation) | Rectangular steel archwire, preferably 0.019 × 0.025-in. | Two ways: Directly on the brackets, when they already have hooks; or connection on hooks clipped to the arches, positioned between two brackets. | Stretched to approximately 3 times its original size. 1/8-in medium force elastics for triangles in the canine region, 3/8-in light or medium force elastics for the M configuration, and 3/16 or 1/4-in medium force elastics for the configuration of triangles with Class II or Class III direction | ||
| Elastics in transverse direction | In the arch in which greater control is desired, the use of a rectangular stainless steel archwire is recommended, whereas in the arch in which greater effect is desired, a thinner archwire can be used. | For buccal cross-bites – bonded buttons on lingual side to brackets on buccal side. Midline correction - Hooks of one side of a particular arch to contralateral side of the opposite arch. |
Cross-bite correction – 1/8-in medium force elastic. Midline correction-3/16-in medium force. |
100 g |
| Connection | Indication | Uses | Force | |
|---|---|---|---|---|
| Anterior elastics | Lower lateral incisor to the upper laterals or central incisor teeth or from the lower cuspid to the upper laterals. | To improve the over bite relationship of incisor teeth. Open bite up to 2 mm may be corrected with these elastics. | Closing spaces between anterior teeth | Force-1–2 oz (28.35–56.7 g) |
| Zigzag elastic | Bicuspid to cuspid and bicuspid to molar. | Extraction cases and where spacing is present. | Rotation correction on the bicuspids. | 2.5 oz (70.87 g) |
| Cross bite elastics | Between the lingual aspect of the lingually placed molar and the buccal aspect of the opposing tooth. | Unilateral and bilateral cross bites. | To expand and upright lower molars which have tipped lingually. | 5–7 ounce (141.75 g–198.45 g) |
| Box elastics | Elastics attached around the maxillary central and mandibular lateral brackets. Lateral boxes attached to maxillary laterals and cuspids and mandibular cuspids and bicuspids. Buccal boxes used to settle in the posterior occlusion or correct a more posterior open bite. | Tooth extrusion and improve intercuspation | To correct the open bite or to decrease the anterior open bite | 1/4” 6 oz or 3/16” 6 oz. (170.1 g) |
| Diagonal elastics | One side upper intermaxillary hook to the other side lower intermaxillary hook | Midline corrections | 1½–2½ ounces (42.52–70.87 g) | |
| Triangular elastics | Upper cuspid to the lower cuspid and first bicuspid teeth. | When a single tooth has to be brought to the occlusion. | It is used for similar reasons of box elastics, but including only 3 teeth. | 1/8” 3½ oz (99.2 g) |
| Vertical elastics (spaghetti) | When there is difficulty in closing the bite, whether anteriorly or posteriorly. | 3½ oz (99.2 g) | ||
| W elastics | In class II vector ‘W’ with a tail is given. | Open bite or c1 III tendency | Occlusal settling | 3/4” 2 ounce (56.7 g) |
| M elastics | The arch wire is sectioned distal to laterals or cuspids and up and down elastics (“M” with a tail) are worn. | Open bite or c1 III tendency | Occlusal settling | 3/4” 2 ounce (56.7 g) |
| Lingual elastics | Class II elastics attached between to lingual hook of the lower molar and intermaxillary hook of upper arch wire on the same side | To upright lingually tipped lower molars. | 1.5–2.5 oz (non-extraction) (42.25–70.87 g) 2–4 oz (extraction) (56.7–113.4 g) | |
| Check elastics | One end of the elastic is hooked over the cinched distal end of the upper arch wire; both strands are hooked under the cinched distal end of the lower arch and the other end on the elastic hook mesial to the canine. | Overbite reduction, causing extrusion of maxillary and mandibular molars and counteracting the tendency of the anchor bends to tip the molars distally plus aiding incisor intrusion | Vertical anchorage | |
| Sling shot elastics | Two hook on buccal and lingual side of the molar to be incorporated in the acrylic plate to hold the elastic. The elastic is stretched at the mesial aspect of molar to distalize it. | Molar distalization | Molar distalization | |
| C1 and C1 pull elastics | The elastic is used between each pair of teeth and hence on the central incisors on opposite sides of the midline | Final setting of teeth | Final setting of teeth | 3/4”, 2 oz (56.7 g) |
ELASTIC FORCES AND FORCE DECAY
In Class II and Class III elastics, the current review and research literature suggest that using light force can be gained by wearing elastics of size 3/16 inches in diameter.[35-37] Forces advised by clinicians were (1–2 ounces (oz),[38,39] 2.5 oz,[40] 3.5 oz,[41] 4 oz,[35] and 6 oz[37]).[42] The rubber bands show a decay of force within 1st h of their placement in the mouth. About 20–25% of force decay is seen within 24 h[43] of which 15% occurs within 1st h. It concludes that the elastics should be changed every day for optimum force delivery to get the desired effect. Force values do get affected by salivary contents and pH, bacteria, forces of mastication, and various foods and temperatures, which cause the rubber to break down due to the formation of a knotty tearing mechanism in its structure, causing it to swell up and, hence, resulting in force decay.[44]
BIOCOMPATIBILITY OF ELASTICS
Latex allergy
It is a medical term which involves the range of allergic reactions to the proteins present in natural rubber latex.[45] Cutaneous exposure of individuals sensitive to latex frequently causes contact dermatitis, stomatitis with acute swellings, and erythematous buccal lesions.[46] Latex allergic incidents in orthodontics increase the use of non-elastic products within the orthodontic practice as well as the assessment of materials’ physical properties of non-latex elastics, which will become increasingly important during clinical practice.[9]
The common undesired effects, from the improper use of elastics are – extrusion of the lower first molar, steepening of the occlusal plane, extrusion of the upper incisors, and flaring of the lower incisors. Some of the above negative effects could be prevented by the use of cortical anchorage, or skeletal anchorage. Absolute or skeletal anchorage can be achieved using TADs.
The extrusion of the maxillary incisors, with the consequent reduction of their torque, and the bite deepening, produces a gummy smile. This could be prevented using sectional mechanics that consist of the cutting of the maxillary arch wire at the level of the upper canine, thereby excluding the maxillary incisors from the traction made by the elastics. These two sections, obtained, could be effective in transferring the force applied to the canine directly to the maxillary molars. Furthermore, intrusion bend can activate the sections that produce around 50 g of force, which will prevent the extrusion of the canine as given by the vertical component of the elastic pull.[47]
CLINICAL IMPLICATIONS
A number of variables are responsible for the effective tooth movement while using intermaxillary elastics, namely, volume and density of bone, patient’s growth phase, previous trauma or current pathology, length, number, surface area of roots, and their individual anatomy. All these can alter the force levels along with modifications of placing the elastics such as single elastic use, double elastics usage, or to increase the initial stretch, adding an extra tooth in the group. Some articles found that daytime wear of elastics has a greater degree of vertical component due to the stretching of the mouth in a range of 10–25 mm, while at night, both horizontal and vertical components are approximately equal. The force levels also depend on the required tooth movement and its direction. Maintenance of hygiene is a very important aspect of using elastics as it is proven in the literature that latex causes a high amount of hygiene issues due to the accumulation of plaque; hence, changing of elastics every day or every 24 h.
CONCLUSION
Without any doubt, intermaxillary elastics are the most important aspect of orthodontic treatment due to their wide possibility and versatility of biomechanical application. However, clinically, it is most important to have a thorough knowledge of the desired effects and of the possible negative effects that are normally associated with the biomechanics using elastics so that the results are obtained as planned and desired by the orthodontist.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Biomechanics and esthetic strategies in clinical orthodontics Netherlands: Elsevier Health Sciences; 2005.
- [Google Scholar]
- Force decay evaluation of latex and non-latex orthodontic intraoral elastics in vivo study. Dent Press J Orthod. 2018;23:42-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and biomechanical considerations of elastics in orthodontics. R Clin Ortodon Dental Press. 2006;5:44-57.
- [Google Scholar]
- An in vitro comparison of 4 brands of nonlatex orthodontic elastics. Am J Orthod Dentofacial Orthop. 2003;123:401-7.
- [CrossRef] [PubMed] [Google Scholar]
- Force decay of latex and non-latex intermaxillary elastics a clinical study. Eur J Orthod. 2016;38:39-43.
- [CrossRef] [PubMed] [Google Scholar]
- In vitro assessment of the mechanical properties of latex and non-latex orthodontic elastics. Am J Orthod Dentofacial Orthop. 2001;120:36-44.
- [CrossRef] [PubMed] [Google Scholar]
- Cytotoxicity of latex and non-latex orthodontic elastomeric ligatures on L929 mouse fibroblasts. Br Dent J. 2010;21:205-10.
- [CrossRef] [PubMed] [Google Scholar]
- The philosophy of the tooth positioning appliance. Am J Orthod Oral Surg. 1945;31:297-304.
- [CrossRef] [Google Scholar]
- Light force technique combining the sliding section and laminated arches. Am J Orthod. 1966;52:85-102.
- [CrossRef] [PubMed] [Google Scholar]
- An updated systematic review regarding early Class II malocclusion correction. J World Fed Orthod. 2019;8:89-94.
- [CrossRef] [Google Scholar]
- Comparison of AdvanSync and intermaxillary elastics in the correction of Class II malocclusions a retrospective clinical study. Am J Orthod Dentofacial Orthop. 2016;150:979-88.
- [CrossRef] [PubMed] [Google Scholar]
- Biomecânica aplicada à clínica In: Elásticos ortodônticos. Maringá: Dental Press; 2013. p. :85-116.
- [Google Scholar]
- Elastics in orthodontics: behavior and clinical application. Rev Dent Press Ortodon Ortop Maxilla. 2003;8:115-29.
- [Google Scholar]
- Compensatory treatment of Class II malocclusion with the use of intermaxillary elastics. Clinical Journal of Orthodontics Dental Press. 2016;15:74-84.
- [Google Scholar]
- Correction of Class II malocclusion with Class II elastics a systematic review. Am J Orthod Dentofacial Orthop. 2013;143:383-92.
- [CrossRef] [PubMed] [Google Scholar]
- Class II non-extraction patients treat-ed with the forsus fatigue resistant device versus intermaxillary elastics. Angle Orthod. 2008;78:332-8.
- [CrossRef] [PubMed] [Google Scholar]
- Attractiveness of the facial profile comparison of Class II patients treated with Twin Force(r) or intermaxillary elastics. Dental Press J Orthod. 2021;26:e212014.
- [CrossRef] [PubMed] [Google Scholar]
- Intermaxillary elastics: Which one to choose and when to ask the patient to change them? (Doctoral dissertation, Baylor College of Dentistry-Dallas, TX) 2016.
- [Google Scholar]
- Therapeutic changes in the occlusal plane inclination using intermaxillary elastics. J Orofac Orthop. 2012;73:377-86.
- [CrossRef] [PubMed] [Google Scholar]
- Current orthodontic concepts and techniques (2nd ed). Toronto: W.B. Sounders Company; 1975.
- [Google Scholar]
- Lexicon universal encyclopedia New York, USA: Lexicon Publication Inc; 1987. p. :332-4.
- [Google Scholar]
- History of orthodontic braces and orthodontia. Available from: https://www.roederorthodontics.com [Last accessed on 2016 Apr 09]
- [Google Scholar]
- Synthetic elastomeric chains a literature review. Am J Orthod Dentofac Orthop. 1994;105:536-42.
- [CrossRef] [PubMed] [Google Scholar]
- A brief history of orthodontics. Am J Orthod Dentofac Orthop. 1990;98:176-82.
- [CrossRef] [PubMed] [Google Scholar]
- Forces produced by orthodontic elastics as a function of time and distance extended. Eur J Orthod. 1986;8:198-201.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontic biomechanics with intermaxillary elastics. In: Dental Press J Orthod. Vol 28. 2023. p. :e23spe3.
- [CrossRef] [PubMed] [Google Scholar]
- Elastics and elastomeric in orthodontics practice. Int J Prev Clin Dent Res. 2018;5:S21-30.
- [Google Scholar]
- Dentoskeletal and soft-tissue changes in growing class II malocclusion patients during nonextraction orthodontic treatment. SADJ. 2006;61:344-50.
- [Google Scholar]
- Correction of class II malocclusion with class II elastics: A systematic review. Am J Orthod Dentofac Orthop. 2013;143:383-92.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontic: Current principles and techniques (5th ed). Netherlands: Elsevier; 1994.
- [Google Scholar]
- Overjet reduction and molar correction in fixed appliance treatment of class II, division 1, malocclusions: Sagittal and vertical components. Am J Orthod Dentofacial Orthop. 1999;115:13-23.
- [CrossRef] [PubMed] [Google Scholar]
- “Effective” TMJ and chin position changes in Class II treatment: orthodontics versus orthopedics. Angle Orthod. 2008;78:813-8.
- [CrossRef] [PubMed] [Google Scholar]
- Two different applications of Class II elastics with nonextraction segmental techniques. Angle Orthod. 2007;77:694-700.
- [CrossRef] [PubMed] [Google Scholar]
- Orthodontics: Diagnosis and management of malocclusion and dentofacial deformities, E-book Netherlands: Elsevier Health Sciences; 2019.
- [Google Scholar]
- Elastics selector gauge as orthodontics device applied to inter-maxillary traction during malocclusion correction. J Funct Morphol Kinesiol. 2019;4:63.
- [CrossRef] [PubMed] [Google Scholar]






