Translate this page into:
Diode laser-assisted excision of mucocele: A case series
*Corresponding author: Anshika Dixit, Department of Pediatric Dentistry, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. dikshitanshika96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dixit A, Gupta A, Das D, Navit S. Diode laser-assisted excision of mucocele: A case series. Asian J Oral Health Allied Sci. 2024;14:14. doi: 10.25259/AJOHAS_9_2024
Abstract
Mucocele is one of the most common lesions of the oral mucosa which occur through mucus secretion accumulations. These mucous build-ups are mostly caused through lip biting habits, trauma, or changes in minor salivary duct function. The most common site of mucocele lesions is the lower lip in the oral cavity. Although mucoceles do not exhibit any age predilection, they mostly affect young patients. Their diagnosis is primarily clinical due to the pathognomonic appearance of mucocele. Based on histological findings, they are two types – extravasation and retention. There are many ways of excising a mucocele, off which laser diode-assisted excision promotes adequate healing of the site and decreases the possibility of its recurrence. Here is a case series of children with mucocele treated with laser-assisted excision.
Keywords
Lower lip
Mucous
Salivary glands
Laser assisted excision
INTRODUCTION
Mucocele cystic formations are benign and occur when mucus accumulates, leading to “mucus-filled cavities”. Mucus accumulation can happen in different parts of the body like in the mouth, appendix, gall bladder, paranasal glands, or lacrimal sac. Mucocele is derived from the Latin words mucus meaning mucus and coele meaning cavity.
Mucoceles are the most frequent conditions affecting the small salivary glands, usually showing up as solitary, bluish, or see-through lumps that are usually asymptomatic, particularly on the lower lip. Mucous cyst is the second most frequent lesion in the mouth, after irritational fibroma.[1] It mostly occurs in young individuals, with 70% of them being younger than 20 years when small salivary duct changes occur. There are two kinds of mucocele: Extravasation and retention. For children, extruded mucocele, i.e., the extravasation type is the most frequent, whereas retention is exceedingly uncommon.[2] Extrusion happens when a damaged salivary gland duct leads to mucus seeping into the nearby soft tissues. There are three evolutionary phases to this process. The initial phase is when mucus escapes from the duct into the surrounding connective tissues. The second phase involves the granuloma formation as a response to a foreign body. The final phase is when a pseudo-capsule forms around the mucosal layer without any epithelial cells. On the other hand, retention mucocele happens from the obstruction of salivary glands.[3]
Extravasation and retention mucoceles are similar in clinical findings. They show up as bluish, tender, see-through lumps that often resolve by themselves.[4,5] The bluish hue comes from blood congestion, cyanosis of the tissue above, and contents of the fluid. Yet, the hue can vary based on the size of the lesion, the area it covers, and elasticity of the overlying tissue.[6]
Extravasation mucoceles are typically seen on the lower lip, with the tongue coming next, followed by the mucosa of the buccal palate, and very rarely on the retromolar area.[7] On the contrary, retention mucoceles can be found throughout the oral cavity.[8] If they are seen at the floor of the mouth, they are known as ranulas due to their resemblance to a frog’s belly.[4]
Often, mucoceles do not lead to any noticeable signs or symptoms. Yet, occasionally, they may result in challenges with speaking, eating, or swallowing. The different surgical methods for treating mucoceles are surgical removal, marsupialization, micromarsupialization, cryosurgery, and laser vaporization, as well as laser removal.[5] The diode laser stands out as a top-notch laser for soft-tissue operations. It shows a decent affinity to pigments (such as hemoglobin), which means it has good hemostatic capability. These lasers are not very absorbed by the teeth, allowing for soft tissue operations to be done near the enamel, dentin, and cementum without risk. Their compact size, portability, efficient cutting ability, and relatively affordable price points are their key benefits. Along with all its cons, however, diode lasers should be used judiciously to avoid harmful irreversible effects over the mucosa.
In this article, we will look at a series of cases of lower lip mucocele treated with laser-assisted excision.
CASE SERIES
Case 1
A 10 year-old-boy came to the Department of Pediatric Dentistry, Saraswati Dental College and Hospital, Lucknow, with a painless swelling in the inner part of the lower lip for three weeks. The swelling started small and gradually increased to the current size. The boy had no relevant medical history.
Intraoral examination revealed a round, isolated, and variable swelling on the inner surface of the lip at the right center incisor. The swelling was 1–2 mm below the lower lip’s vermilion border and was approximately 8 mm in diameter [Figure 1a]. The color of the swelling matched the color of the surrounding mucosa. There were no other oral abnormalities. Speech and chewing were not affected. A differential diagnosis of mucocele, oral hemangioma, oral lympangioma, lipoma, and soft tissue abscess was made.

- (a) A 10-year-old boy with mucocele in the left side of lower lip, (b) diode laser-assisted excision of the mucocele, (c) immediate post-operative photograph after the excision of the mucocele, (d) post-operative photograph of follow-up after one week during the healing phase.
Based on the clinical characteristics, the lesion was classified as Mucocele and its excision was planned. To control pain during mucocele excision, topical lignocaine gel 2% (Lox 2%, Neon Laboratories Ltd, India) was applied over the site for 2 min, followed by infiltration of 1 mL of local anesthesia with insulin syringe (Dispovan, Hindustan Syringes and Medical Devices Ltd., Haryana) of 31 gauge (i.e. 0.25 × 6 mm) around the periphery of the lesion. The local anesthetic used was 2% lignocaine with 1:80,000 adrenaline (Lignox 2% A, Indoco Remedies Ltd., India). The lesion was then excised using soft tissue diode laser (Ezlase®, Biolase Technology Inc., Irvine, California) of wave length 940 nm at in-built “Excision” preset with CP1 (CP = Comfort Pulse) mode using 400 µm diameter tip [Figure 1b and c]. The details of the parameters used for the mucocele excision in CP1 mode are mentioned in Table 1.
| Preset Name | Excision |
|---|---|
| Wavelength | 940 nm |
| Average power | 0.9 W |
| Peak Power | 2.7 W |
| Duty cycle | 30% |
| Pulse duration | Pulse interval-0.2 ms Pulse length-0.1 ms |
| Energy (Pulse energy) | 9×10−5J |
| Emission mode | Pulse mode |
| Method (contact/non-contact) | Contact |
| Tip size | 400 µm |
| Angulation | Tip perpendicular to the tissue in a sweeping motion |
| Irradiation duration | 7 min |
| Power density | 1830 W/cm2 |
| Fluence | 0.071 J/cm2 |
Both the operator and the patient undergoing the procedure donned the protective eyewear. The mucocele and the surrounding oral mucosa were sterilized with 5% povidone-iodine (Microgen Hygiene Pvt. Limited, Maharashtra) before surgery [Figure 1b]. The tip was gently applied perpendicular to the tissue at the base of the lesion and was used in a sweeping motion. The area was meticulously mopped by sterile wet gauze to prevent the mucosa from overheating. If any accumulation of debris was noticed over the tip during the procedure, the tip was carefully cleaned with a sterile gauze. Once the lesion was excised the operative field was wiped with a sterile gauze soaked in 1% normal saline. The mucocele was completely removed within 7 min. There was no bleeding at the site and no stitches were required. The specimen was subjected to histopathological examination and showed parakeratinized stratified squamous epithelium underlying the moderately dense and inflamed connective tissue stroma with minor salivary glands. Cystic space was observed within the stroma which was lined by dense and inflamed (lymphocytes, neutrophils, and macrophages) capsule. Many small endothelial-lined blood vessels are seen within the stroma. Mucous salivary glands are also observed adjacent to cystic space which is infiltrated by inflammatory cells. With all these histopathological features, diagnosis of mucocele was established. The patient was advised not to consume hot, spicy food and was prescribed non-steroidal analgesic, Flagyl Dental Gel (Abbott India Ltd., Mumbai) and 0.2% chlorhexidine mouthwash 2–3 times/day for a period of 7 days. The patient was also advised to avoid biting the lower lip to avoid its recurrence. At a week’s follow-up, healing was uneventful [Figure 1d]. At one-month follow-up, there was minimal scarring at the site while at three-month follow-up, scarring at the site disappeared without any recurrence of the lesion.
Case 2
An 18-year-old girl reported to the department with the complaint of swelling on left side of the lower lip, near the oral commissure, after the trauma one year back. The swelling was similar in color to the adjacent mucosa, soft to firm in consistency, and round in shape, measuring approximately 9 mm in diameter [Figure 2a]. It was diagnosed as mucocele based on history and clinical appearance. Surgery was performed under local anesthesia (technique and the local anesthesia used being similar to Case Report 1) using diode laser (Ezlase®, Biolase Technology Inc., Irvine, California) of 940 nm wavelength to remove the lesion [Figure 2b and c]. The parameters and the precautions taken during the procedure along with the medications prescribed were similar to the Case Report 1. Specimen was sent for histopathological examination and revealed parakeratinized stratified squamous epithelium with underlying moderately dense and loosely arranged connective tissue stroma. The epithelium showed sebaceous glands at few focal areas. The stroma is composed of plum of spindle-shaped fibroblasts, endothelial lined blood vessels, and inflammatory cells chiefly composed of neutrophils and macrophages. The deeper stroma is composed of longitudinally sectioned muscle bundles and mucin pooled cystic spaces infiltrated with neutrophils. Adipose tissue was also appreciated at a few focal areas. These histological features confirmed the diagnosis of mucocele. The healing was evident and uneventful on follow-up of one week [Figure 2d]. At one-month follow-up, there was minimal scarring at the site while at three-month follow-up, scarring at the site disappeared with no recurrence.
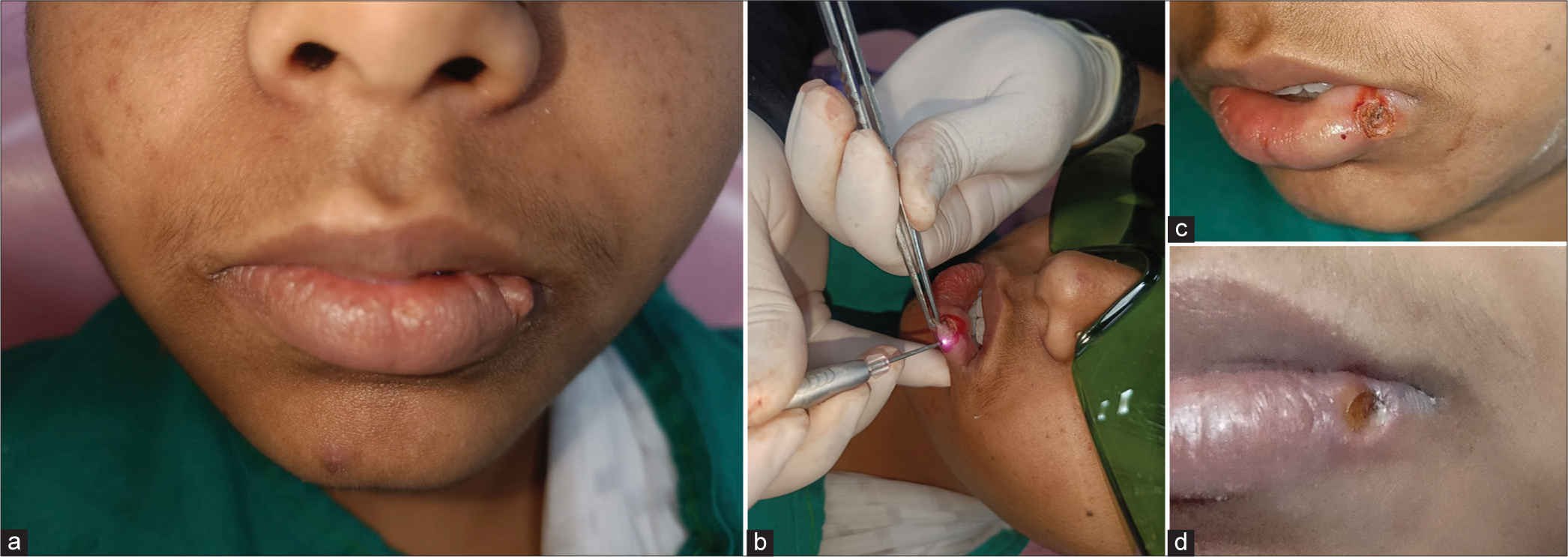
- (a) An 18-year-old girl with mucocele in the left side of lower lip, (b) Diode laser-assisted excision of the mucocele, (c) immediate post-operative photograph after the excision of the mucocele, (d) post-operative photograph of follow-up after one week during the healing phase.
DISCUSSION
A mucocele is a harmless cyst filled with mucus. These cysts are typically painless and appear as round smooth growths. These growths typically give off a bluish, see-through color that can range from 1 mm to 2 mm to several centimeters. The lower lip is the most frequent location for the development of mucocele, followed by the buccal mucosa and floor of the mouth,[6] appearing at rates ranging from 0.4% to 0.9%, with no discernible preference for any gender. At the same time, Wu et al. found that approximately 11.6–21.8% of oral biopsies taken from children contained mucoceles.[7] Even though an oral mucocele is not dangerous, it can develop into a lasting lump at the site of occurrence if left untreated. Mucoceles have a pathognomonic appearance. Around 75% of the lesions measure <1 cm across, but occasionally, their dimensions can range from a few millimeters to several centimeters long. Superficial lesions appear bluish or transparent, while those deeper in the tissue maintain their natural pink color and may bleed into the swelling, giving them a reddish and vascular appearance. The traits that characterize a mucocele include its exact location, any history of injury, its swift development, the variation in size, the bluish hue, the fluid’s consistency, medical background, and observable symptoms, which typically point to a mucocele, among others, such as a lip lipoma, a mucus retention cyst, a minor salivary gland tumor, and various others, all of which manifest as bulges on the lip. However, these conditions, while sharing the lip’s proximity, can be differentiated by their visual presentation, color, texture, cause, and specific location. The characteristics of mucoceles can vary based on their size and position, leading to symptoms such as external enlargement, difficulty in chewing, swallowing, and speaking, and possible discomfort. Analysis of mucocele through histopathology frequently shows the formation of clearly defined, cyst-like areas encircled by granulation tissue, along with the detection of mucinophages within the ruptured wall of granulation tissue.[8] Among the different methods for treating mucocele, laser excision stands out as a leading technique. The primary benefits of using soft-tissue lasers include reduced bleeding and swelling, less post-operative pain, and minimal scarring and coagulation, no requirement for sutures because the natural healing process is aided by the denatured proteins in the wound. The case described here utilized a wavelength of 940 nm, which proved effective in achieving hemostasis thanks to its strong affinity to pigments such as hemoglobin.[9] Diode lasers offer a practical substitute for bigger surgical lasers such as erbium-doped yttrium aluminum garnet laser and carbon dioxide lasers. They provide a precise cutting edge, along with the ability to coagulate and hemostasis during excision. During laser excision, the lesion needs to be cut through to the muscular layer, all nearby glandular acini and if required the accessory salivary gland should also be eliminated to reduce the chance of recurrence.[10] When laser energy is absorbed by the target tissue, it generates heat through a photothermal process. This heat then leads to the vaporization of cells with resultant cellular explosion and tissue ablation. Surrounding tissues also heat up over time with the laser’s application. The thermal impact of the laser can either be reversible or irreversible, resulting in a zone of tissue damage known as coagulation necrosis. Delayed healing and a larger wound area can result from increased duration in laser application. However, the laser can also effectively seal small blood vessels instead of the coagulation necrosis zone, offering benefits such as hemostasis during surgery. The areas near the coagulation ends bleed less at the surgical site.[11] Considering these, it is evident that diode laser excision of mucocele is one of the best methods for mucocele removal which ensures adequate healing of the site and also decreases the possibility of its recurrence. While most of the published case reports used 940 nm diode laser in continuous mode, while in the present case report, excision of the mucocele has been performed in CP1 mode.
CONCLUSION
Management of mucocele is a challenging task due to the high chances of recurrence of such case. Laser excision is among the top methods used to treat mucocele. This procedure helps to decrease tissue loss in the mucosa, lowers the chance of forming extensive scar tissue, and stops the contents of the cyst from leaking out, which could cause the condition to return.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consents.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Excision of mucocele using diode laser in lower lip. Case Rep Dent. 2016;2016:1746316.
- [CrossRef] [Google Scholar]
- An appraisal of oral mucous extravasation cyst case with mini review. J Adv Med Dent Sci Res. 2014;2:166-70.
- [Google Scholar]
- Treatment of lower lip mucocele with diode laser-a novel approach. Ann Dent Res. 2013;2(Suppl 1):102-8.
- [Google Scholar]
- Treatment of lower lip mucocele with Er, Cr: YSGG laser--a case report. J Oral Laser Applic. 2010;10:181-5.
- [Google Scholar]
- Mucoceles of the oral cavity in pediatric patients. Kaohsiung J Med Sci. 2011;27:276-9.
- [CrossRef] [Google Scholar]
- Clinical and immunohistochemical characteristics of mucoceles. Ann Dermatol. 2009;21:345-51.
- [CrossRef] [Google Scholar]
- Laser vaporization of extravasation type of mucocele of the lower lip with 940-nm diode laser. Indian J Dent Res. 2013;24:278.
- [CrossRef] [Google Scholar]
- Oral mucoceles in children-analysis of 56 new cases. Pediatr Dermatol. 2015;32:647-50.
- [CrossRef] [Google Scholar]
- Laser applications in oral and maxillofacial surgery. Implant Dent. 1997;6:238.
- [CrossRef] [Google Scholar]






