Translate this page into:
Custom healing abutments: A practical approach for deep subgingival implants
*Corresponding author: Priya Hemant Mishra, Department of Prosthodontics and Crown & Bridge, Saraswati Dental College and Hospital, Lucknow, Uttar Pradesh, India. priya8179hm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mishra PH, Srivastava P, Chopra D, Yadav P. Custom healing abutments: A practical approach for deep subgingival implants. Asian J Oral Health Allied Sci. 2025;15:3. doi: 10.25259/AJOHAS_20_2024
Abstract
This case study describes the rehabilitation of a missing maxillary anterior tooth using a customized gingival healing abutment for a deeply placed implant, focusing on optimal esthetics and function. Rehabilitating missing anterior teeth is challenging due to the need for precise esthetics and functional integration. Deeply placed implants complicate soft-tissue management and emergence profile, making customized gingival healing abutments essential for achieving satisfactory outcomes. A 59-year-old male presented with a missing maxillary anterior tooth. After implant placement, a deeply positioned implant was identified. A customized gingival healing abutment was fabricated to shape the soft tissue and create a natural emergence profile. After healing, a cement-retained prosthetic crown was placed, resulting in satisfactory fit, esthetics, and patient satisfaction. The use of customized gingival healing abutments is crucial in prosthodontic rehabilitation of deeply placed implants, especially in esthetically sensitive areas. This approach improves patient satisfaction and treatment success.
Keywords
Customized gingival healing abutment
Deeply placed implant
Implant-transfer piece
Soft-tissue management
INTRODUCTION
Rehabilitation of missing anterior teeth, especially in the maxillary region, presents a unique challenge due to the high esthetic demands and the need for functional harmony. Implants have become the preferred treatment option for such cases, providing a stable and long-lasting solution. However, when implants are placed deeply within the alveolar bone, several challenges arise, particularly concerning the management of soft-tissue contours and the creation of an appropriate emergence profile.[1]
A deeply placed implant often results in insufficient soft-tissue height and volume around the implant site, which can lead to compromised esthetics if not properly addressed. Traditional healing abutments, while effective in maintaining the implant’s soft-tissue interface, are typically designed with a uniform cylindrical or conical shape. This generic design does not mimic the natural contour of the gingiva, resulting in inadequate soft-tissue shaping. Consequently, they often fail to establish the complex three-dimensional architecture required to support a natural and harmonious emergence profile, particularly in esthetically sensitive regions. Such limitations can lead to soft-tissue irregularities and an unnatural appearance of the final prosthesis.[1]
In contrast, a customized gingival healing abutment becomes essential in these cases. This abutment is specifically designed to replicate the natural contours of the gingiva, guiding the healing process to achieve a more natural and esthetically pleasing outcome. The design and use of a customized gingival healing abutment allow for precise control over the soft-tissue architecture, promoting better integration with the final prosthesis.[2] This approach is particularly important in the maxillary anterior region, where even minor discrepancies in soft-tissue contours can significantly impact the esthetic outcome.[3] By carefully shaping the gingiva during the healing phase, clinicians can ensure that the final restoration blends seamlessly with the surrounding natural dentition, providing both functional and esthetic satisfaction.
CASE REPORT
A 59-year-old male patient visited the Department of Prosthodontics at Saraswati Dental College with a chief complaint of missing teeth in the maxillary anterior region. The patient had a history of tooth loss in this area and had previously undergone implant placement. Clinical examination and radiographic evaluation revealed a deeply placed implant at the site, i.e., 21 regions (Osstem, South Korea, UCK, TS system implant, −3.0 × 10 mm [Figure 1]). To address the esthetic and functional challenges, a customized gingival healing abutment was designed and fabricated. This abutment was used to shape the soft tissue and create a natural emergence profile. After adequate healing, the patient was rehabilitated with a cement-retained prosthetic crown on the implant. The final prosthesis was evaluated for fit, esthetics, and patient satisfaction.
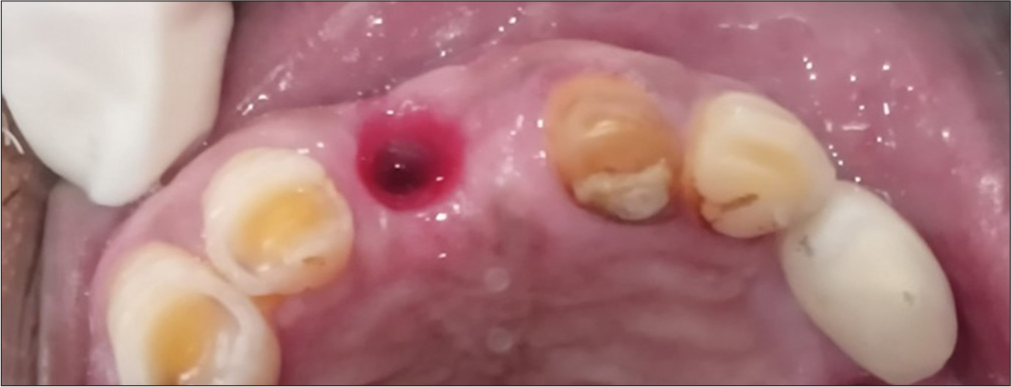
- Subgingival (deeply) placed implant.
Technique
The optimum length of the prefabricated healing abutment was determined using a calibrated Vernier calliper for precise measurement [Figure 2a]. This prefabricated healing abutment served as the base for creating a customized version tailored to the patient’s soft tissue requirements [Figure 2b]. Circumferential retentive grooves were incorporated into the prefabricated abutment to enhance the bonding of composite material. The surface was sandblasted with 50 mm aluminium oxide to increase micromechanical retention. Following sandblasting, a metal primer (Alloy Primer, Kuraray Medical Inc., Okayama, Japan) and bonding agent (Clearfil SE Bond, Kuraray Medical Inc.) were applied to promote chemical adhesion.
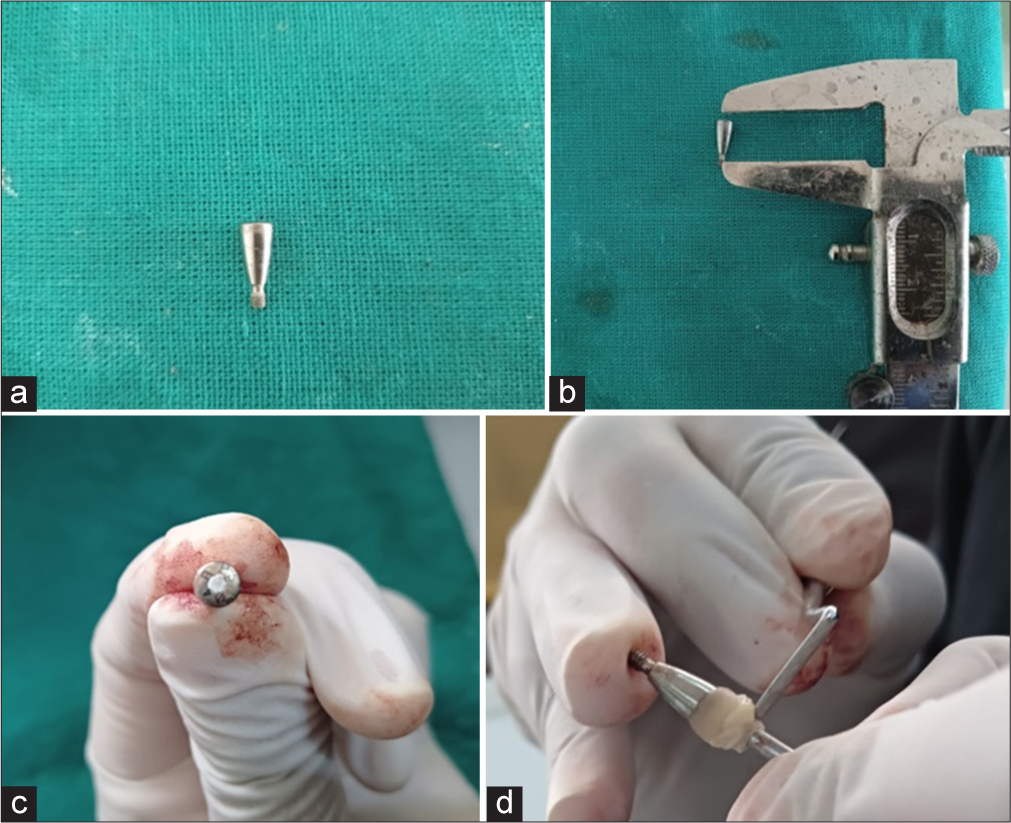
- (a) Prefabricated healing abutment, (b) calibrated Vernier calliper for precise measurement, (c) screw access hole sealed with Teflon tape, (d) composite resin was applied circumferentially around the prefabricated healing abutment extraorally.
To create the customized healing abutment, the screw access hole was sealed with Teflon tape [Figure 2c] to prevent composite resin from entering. Flowable composite resin (Clearfil Majesty Flow, Kuraray Medical Inc.) was applied circumferentially around the prefabricated healing abutment extraorally. The composite was shaped to mimic the desired emergence profile. During this process, the material was added in thin, controlled layers to ensure uniformity, with polymerization after each layer to maintain structural stability. Excess material was carefully removed using a fine rotary instrument to achieve the desired contour and a smooth finish [Figures 2d, 3a and b].
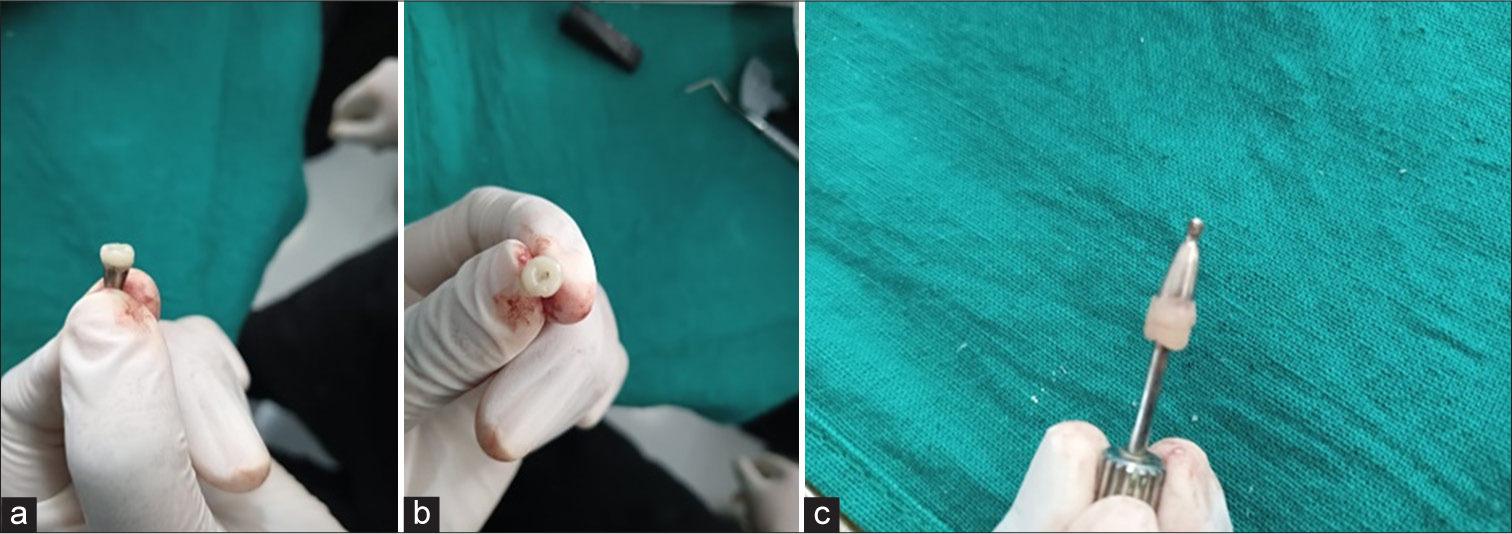
- (a) Side (lateral) view of the abutment shaped to mimic the desired emergence profile, (b) top view of the abutment shaped to mimic the desired emergence profile, (c) final customized healing abutment extended 4 mm long.
The final customized healing abutment was designed to extend 4 mm longer than the longest prefabricated healing abutment available in the implant system. This extension provided optimal support for soft-tissue shaping and the emergence profile [Figure 3c]. Once the desired contour and length were achieved, the composite resin was polished using appropriate burs, following standard procedures to ensure a smooth surface for soft-tissue contact [Figure 4a].
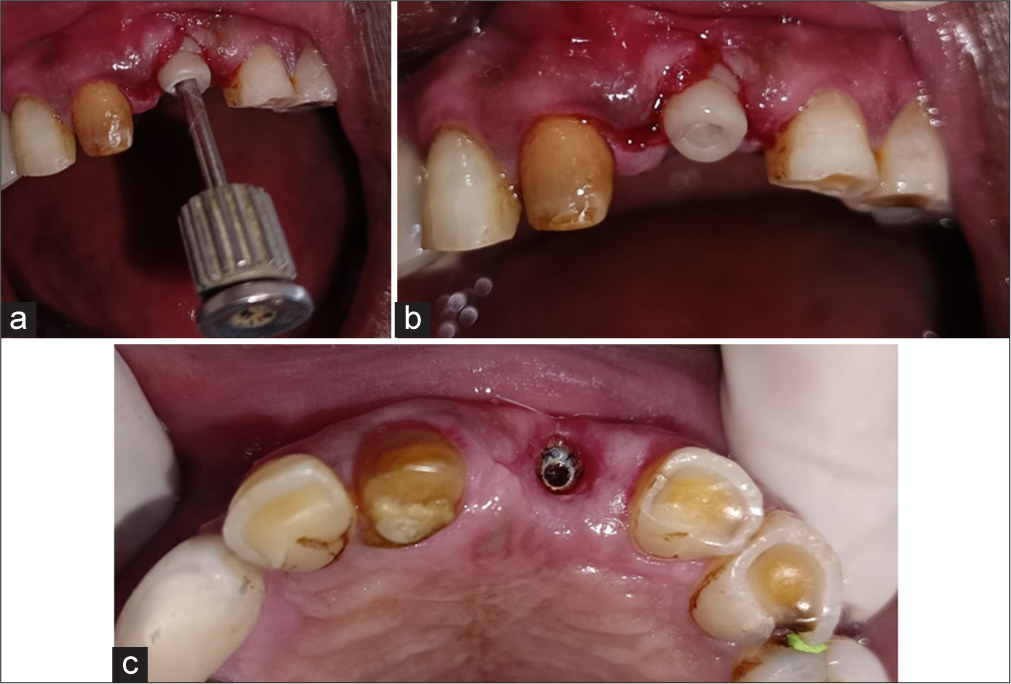
- (a) customized healing abutment placed to ensure a smooth surface for soft-tissue contact, (b) custom healing abutment was secured and torqued using a handheld torque wrench, (c) soft-tissue profile after 1-week follow-up through the customized abutment.
Upon completion, the implant analog was removed, and the custom healing abutment was secured and torqued to 15 N-cm using a handheld torque wrench [Figure 4b]. A follow-up examination was conducted after one week to assess the soft-tissue profile through the customized abutment [Figure 4c].
DISCUSSION
Deeply placed implants are often associated with thin gingival tissue layers, which can pose challenges for achieving ideal esthetics and soft-tissue stability. A thin gingival tissue is more prone to recession and may not provide adequate coverage, leading to compromised esthetic outcomes and difficulty in shaping a natural emergence profile. In such cases, techniques like using a custom-made healing abutment are crucial to optimize the soft-tissue response and enhance the final result. Janakievski[4] discussed a similar approach involving the modification of a temporary abutment used as a healing abutment in the anterior maxilla for immediate post-extraction implant placement. The objective in that case was to achieve an ideal emergence profile for the soft tissue to enhance esthetics. Although a temporary abutment could have been used in our case, it would have incurred additional costs.
Pow and McMilan[1] reported on modifying a healing abutment with polymethylmethacrylate (PMMA) to simulate natural soft tissue and increase the width of the abutment for esthetic purposes, using a standard two-stage surgical protocol to replace a missing maxillary left first premolar. However, their method does not address the need to increase vertical dimension, as required in our case.
Yilmaz et al.[5] described the use of laser welding to elevate the height of a healing abutment for a deeply placed implant. However, we opted not to use laser welding due to its sensitivity, cost, and the need for specialized equipment. As highlighted by Gowda et al., custom-shaped abutments provide the flexibility needed to mold the healing gingival tissue, thereby achieving an ideal emergence profile for permanent restoration.[6] Deep subgingival implant placement often presents challenges in adequately supporting the supracrestal soft tissue, especially when relying on conventional prefabricated healing abutments.
The method detailed in this case report is non-invasive, simple to perform, and yields favorable results. The custom abutment offers several advantages, including ease of fabrication, cost-effectiveness, and enhanced soft-tissue stabilization, all without the need for additional surgical procedures.[7] This approach is particularly beneficial in cases where standard healing abutments are insufficient due to thick gingival tissue or the necessity for deep implant placement. By carefully shaping the gingiva during the healing phase, clinicians can ensure that the final restoration integrates seamlessly with the surrounding natural dentition, achieving both functional and esthetic success.
CONCLUSION
The custom-made healing abutment technique effectively manages deep subgingival implants where conventional abutments fall short due to thick gingival tissue. This tailored approach promotes optimal soft-tissue healing, improving the esthetics and stability of the final restoration. It is a cost-effective, non-invasive alternative to complex methods such as temporary abutments or laser welding, offering significant advantages in challenging implant-supported restorative cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- A modified implant healing abutment to optimize soft tissue contours: A case report. Implant Dent. 2004;13:297-300.
- [CrossRef] [PubMed] [Google Scholar]
- Implant-supported fixed prostheses In: Rosenstiel SF, Land MF, Fujimoto J, eds. Contemporary fixed prosthodontics (4th ed). St. Louis, Mo: Elsevier; 2006. p. :466-504.
- [Google Scholar]
- Effect of subgingival depth of implant placement on the dimensional accuracy of the implant impression: An in vitro study. J Prosthet Dent. 2008;99:107-13.
- [CrossRef] [PubMed] [Google Scholar]
- Case report: Maintenance of gingival form following immediate implant placement-the custom-healing abutment. Adv Esthet Interdisciplin Dent. 2007;3:24-8.
- [Google Scholar]
- A technique to modify the length of an implant healing abutment. J Oral Implantol. 2009;35:201-3.
- [CrossRef] [PubMed] [Google Scholar]
- Peri-implant soft tissue management with customized healing abutments: A case report. J Indian Prosthodont Soc. 2016;16:386-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transfiguration of smile by anterior tooth replacement through remodeling of hard and soft tissue profile with adjunct to implant osseointegration. Contemp Clin Dent. 2022;13:95-8.
- [CrossRef] [PubMed] [Google Scholar]






