Translate this page into:
Management of subgingival proximal defects
*Corresponding author: Rhythm Bains, Department of Conservative Dentistry and Endodontics, King George’s Medical University, Lucknow, Uttar Pradesh, India. docrhythm77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mutalikdesai J, Dhaniba KC, Choudhary S, Verma P, Bains R. Management of subgingival proximal defects: A case series on deep margin elevation. Asian J Oral Health Allied Sci. 2024;14:15. doi: 10.25259/AJOHAS_10_2024
Abstract
Deep proximal cavities can be progressively elevated by a restorative procedure known as deep margin elevation (DME), which improves margins for either direct or indirect restorations. Dietschi and Spreafico (1998) introduced the non-surgical alternative procedure of DME for crown lengthening. Other names for the DME concept include “coronal margin relocation,” “proximal box elevation,” and “cervical margin relocation.” A DME treatment’s therapeutic effectiveness depends on a proper indication, and its clinical efficacy is largely dependent on how well the DME is adjusted. In addition to maintaining periodontal health, a suitable DME adaption may be able to lessen bacterial buildup and the occurrence of secondary caries. Here, we report on three cases of DME that were performed when adequate isolation was possible, and caries was progressing subgingivally.
Keywords
Deep margin elevation
RMGIC
Biologic width
Composite resin
Mineral trioxide aggregate
Subgingival margin
INTRODUCTION
Deep margin elevation (DME) or coronal margin relocation is a method that raises or repositions sub-gingival margins into supra-gingival margins utilizing a range of materials to increase marginal integrity and bonding strength.[1] In 1998, Dietschi and Spreafico presented the DME approach as a solution to sub-gingival restoration difficulties.[2] Clinical dentistry today is focused on conservative, with minimally invasive deep marginal elevation as a viable substitute for more invasive crown lengthening operations in certain circumstances.[3] Anatomical challenges associated with the surgical approach, such as the furcation region, attachment loss, and vicinity to root concavities, could arise. DME deals with a variety of clinical issues related to subgingival margins, which can be difficult to treat due to restricted access, rubber dam slippage over the margin, and the ensuing continuous blood, saliva, and crevice fluid leakage.[1] DME can also be used to improve the marginal seal and bond of indirect adhesive restorations when combined with immediate dentin sealing (IDS). IDS plugs undercut, strengthens undermined cusps, and seals the dentin using an adhesive composite resin base.[4]
CASE SERIES
Following the Preferred Reporting Items for Case Reports in Endodontics (PRICE) 2020 criteria, Flow Chart 1 was created to show the work flow in the cases.
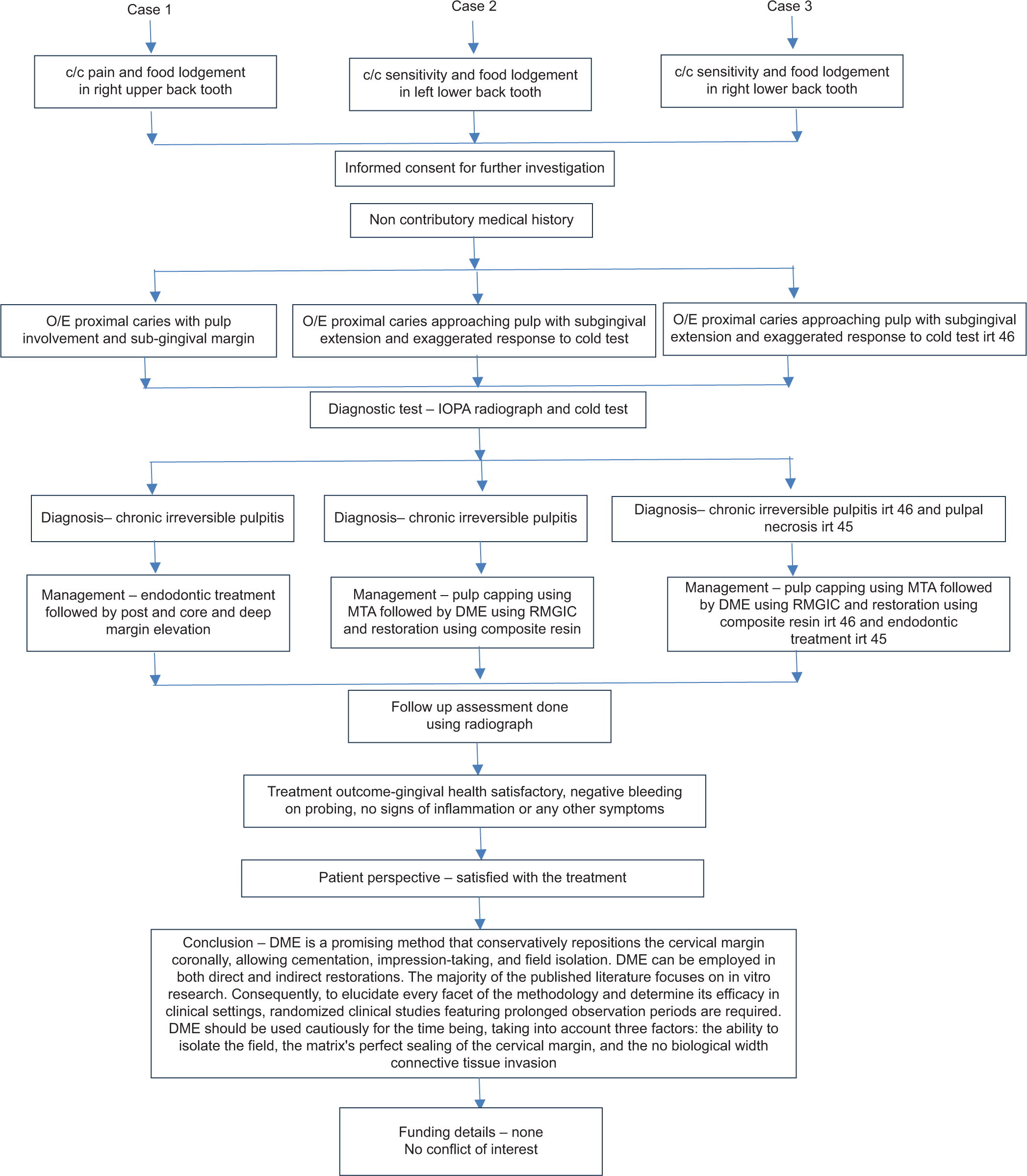
- Flowchart depicting comprehensive management of subgingival defects using DME in case 1, 2 and 3. Case 1- 29 year old female, Case 2 -30 year old male, Case 3- 36 year old male. c/c: chief complaints; O/E: on examination; IOPA: intraoral periapical; MTA: mineral trioxide; DME: deep margin elevation; RMGIC: resin-modified glass ionomer cement; irt: in respect to.
Case 1
A 29-year-old female patient with no significant medical history came to our department, complaining of pain and food lodgment in the right upper back tooth region for 7-8 months. The extraoral examination was normal. On intraoral examination, proximal caries was seen with respect to 14. A radiographic examination revealed proximal caries with pulpal involvement. On caries excavation, more than 50% of tooth structure was lost, with a subgingival extension on the distal side of the tooth. We planned for endodontic treatment followed by post and core with DME. Figure 1 (a-l) depicts the clinical procedures in case 1.
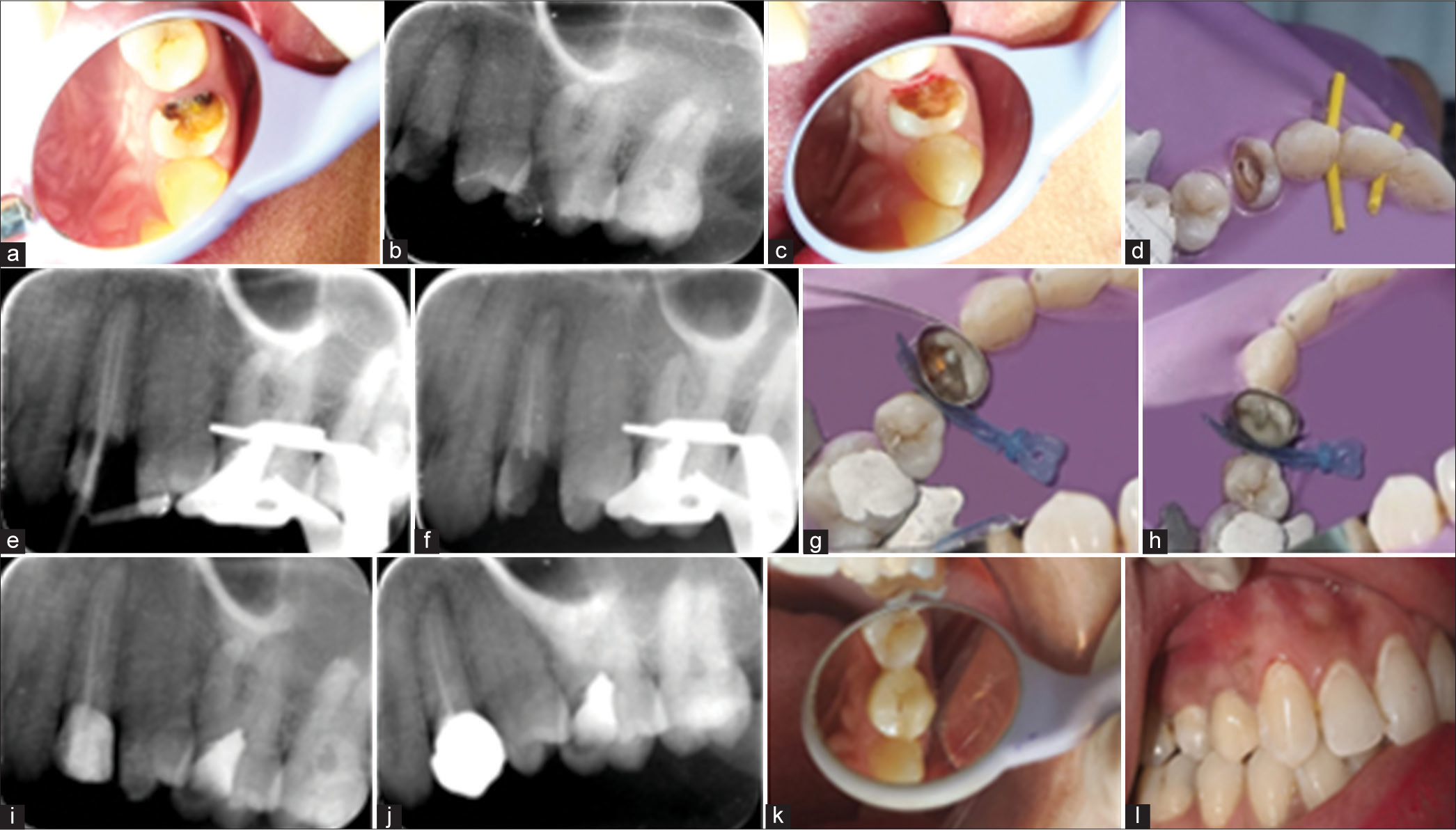
- (a) Pre-operative clinical image, (b) pre-operative radiograph, (c) subgingival marginal after caries removal, (d) access opening, (e) master cone radiograph, (f) obturation (section obturation in palatal), (g) modified matrix system for isolation, (h) fiber post luting and margin elevation done, (i) radiograph after margin elevation. (j) post-operative radiograph, (k) post-operative clinical image, and (l) follow-up clinical image showing healthy periodontium.
Informed consent was taken from the patient. Oral prophylaxis was done before the commencement of treatment. A rubber dam was placed for isolation and protection of soft tissue from any possible chemical or mechanical injury. Complete caries excavation was done using diamond burs. Ultrasonic tips were used to clear off the debris and get clean margins. Access opening was done using Endo access bur and Endo Z bur (Densply, Maillefer, India), patency of the canal was checked using a 10 K file. Working length was recorded using the radiographic method. The apical preparation was made by starting with the first file that binded at the WL. Biomechanical preparation was done with a ProTaper gold NiTi rotary system (Dentsply, Maillefer, India). Irrigation was done in between the mechanical preparation using saline and 1.5% sodium hypochlorite. The canal was dried using a paper point. The master cone was placed inside the canal, and its position was confirmed using a radiograph. AH plus sealer was used. Gutta-percha was seared off using an obturation pen (Endoking, India) and gently condensed into the canal using a hand plugger in the buccal canal, and sectional obturation was done in the palatal canal. Post-space preparation was done with Mani peeso reamer up to size 2 and during post-space preparation, saline irrigation was carried out intermittently. Super endo high-strength glass fiber post of black color (diameter 1.2 mm and length 18 mm) was used. The fiber post was luted using 3M RelyX Universal Resin Cement. Modified matricing (loop was made using a stainless steel matrix band that corresponded to the size of the tooth; it was stabilized using a plastic wedge) was done as the adjacent tooth was rotated. It was difficult to adapt the matrix band securely. Etch-and-rinse adhesives (ERAs) were used. Etching was done using 37% phosphoric acid for 20 s and rinsed with water. Gentle air drying was done, followed by which bonding agent was applied and cured for 30 s. Margin elevation was done using 3M Filtek Z250 XT nanohybrid universal restorative cement (It was used as it is a nanocomposite having the advantage of better dimensional accuracy and mechanical properties). First, a 2 mm increment of the composite was used for margin elevation, followed by which the core buildup was completed. The crown margins on the distal side were placed on the DME, but on the buccal, lingual, and mesial sides, ferrule could be obtained, which was on enamel. Monolith zirconia crown was delivered.
At 1-year follow-up, gingival health was satisfactory, with a probing depth of 2 mm, no signs of inflammation, and no other associated symptoms.
Case 2
A 30-year-old male patient with no significant medical history reported to our department with sensitivity and food lodgment in the lower left back tooth region for 3 months. The extraoral examination was normal. On intraoral examination, proximal caries was seen with respect to 36. Radiograph examination revealed proximal caries approaching the pulp. Cold and electric pulp tests were performed to assess the pulpal response of the teeth. An exaggerated response to the cold test was noted with respect to 36. On caries excavation, subgingival extension was seen on the distal side of the tooth. We planned to do vital pulp therapy with DME. Figure 2 (a-f) depicts the clinical procedures in case 2.
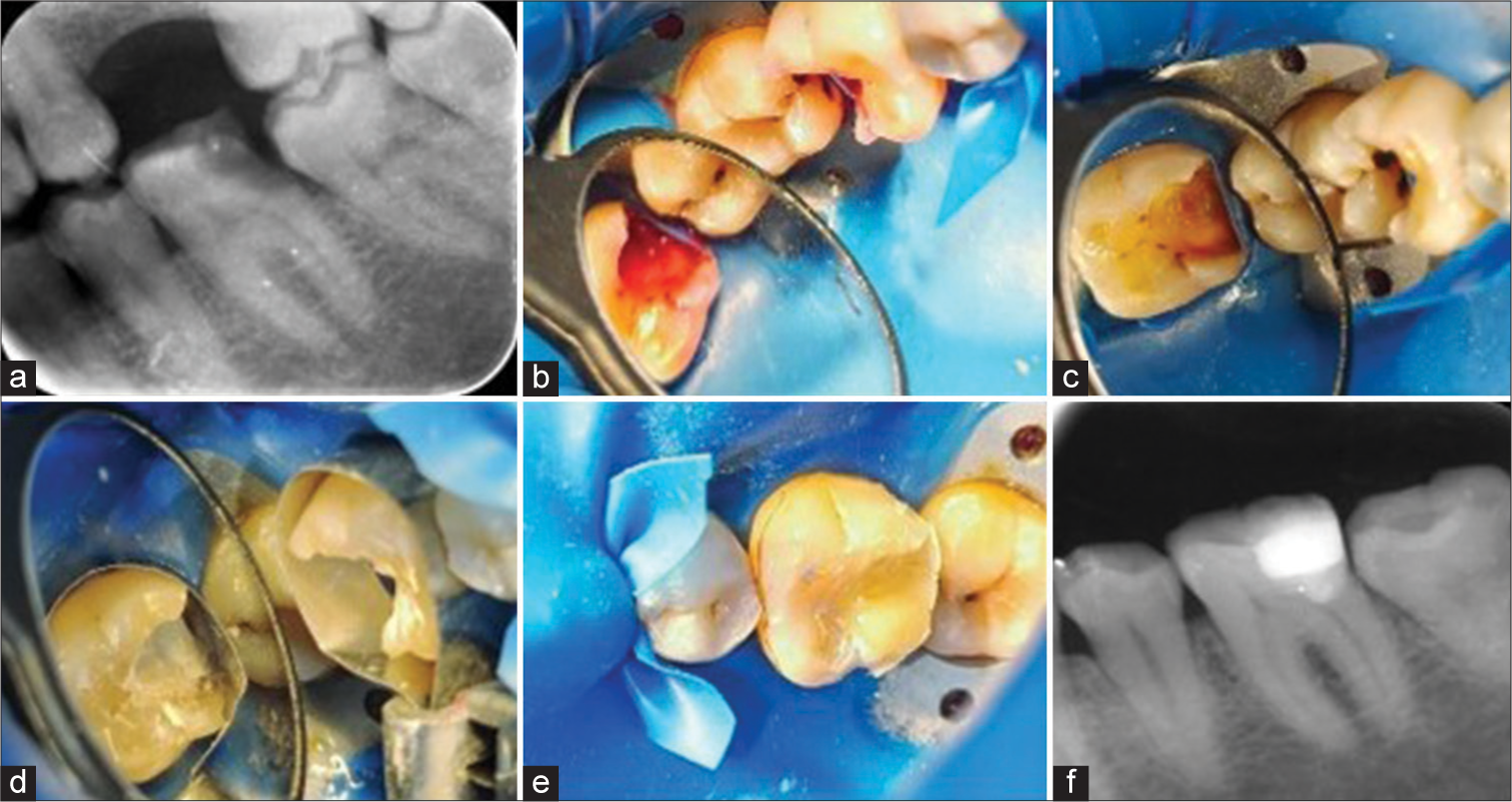
- (a) Pre-operative radiograph, (b) application of caries detection dye, and (c) after complete caries removal, pinpoint pulpal exposure was seen along with subgingival margin. (d) MTA was placed at the exposure site, followed by marginal elevation done using RMGIC, (e) composite restoration done, and (f) post-operative radiograph. MTA: mineral trioxide; RMGIC: resin-modified glass ionomer cement.
Informed consent was taken from the patient. Oral prophylaxis was done before the commencement of treatment. A rubber dam was placed for isolation and protection of soft tissue from any possible chemical or mechanical injury. Gross caries removal was done with No 2 round bur. (Mani, India). One drop of caries detection dye (1% acid red solution in a propylene glycol solvent) was applied using a micro brush and allowed to penetrate for 10 s. It was then rinsed with water and then air-dried. Complete caries excavation was done using diamond burs, and ultrasonic tips were used to clear off the debris and get clean margins. Matricing was done using a pre-contoured sectional matrix (Tor Vm matrix, Filaydent, India). MTA (SafeEndo, India) was mixed according to the manufacturer’s instructions and was placed at the deepest portion of the cavity. Dentine conditioning was done using 10% phosphoric acid before placement of RMGIC. RMGIC (SafeEndo, India) was used for margin elevation. The restoration was done using dental composite resin (3M Filtek Z250 XT Nano Hybrid Universal Restorative cement). It was used as it is a nanocomposite having the advantage of better dimensional accuracy and mechanical properties.
At 1-year follow-up, probing depth of 2 mm, no bleeding on probing was observed. The patient was clinically and radiographically asymptomatic.
Case 3
A 36-year-old male patient with no significant medical history reported to our department with sensitivity and food lodgment in the lower right back tooth region for 3 months. The extraoral examination was normal. On intraoral examination, proximal caries was seen with respect to 46 and 45. Radiograph examination revealed proximal caries approaching pulp with respect to 46 and pulpal involvement with respect to 45. Cold test and electric pulp tests were performed to assess the pulpal response of the teeth. An exaggerated response to the cold test was noted in the first 46, while 45 gave no response. On caries excavation, subgingival extension was seen on the mesial side of the tooth 46. We planned vital pulp therapy with DME with respect to 46 and endodontic therapy with respect to 45. Figure 3 (a-g) depicts the clinical procedures in case 3.
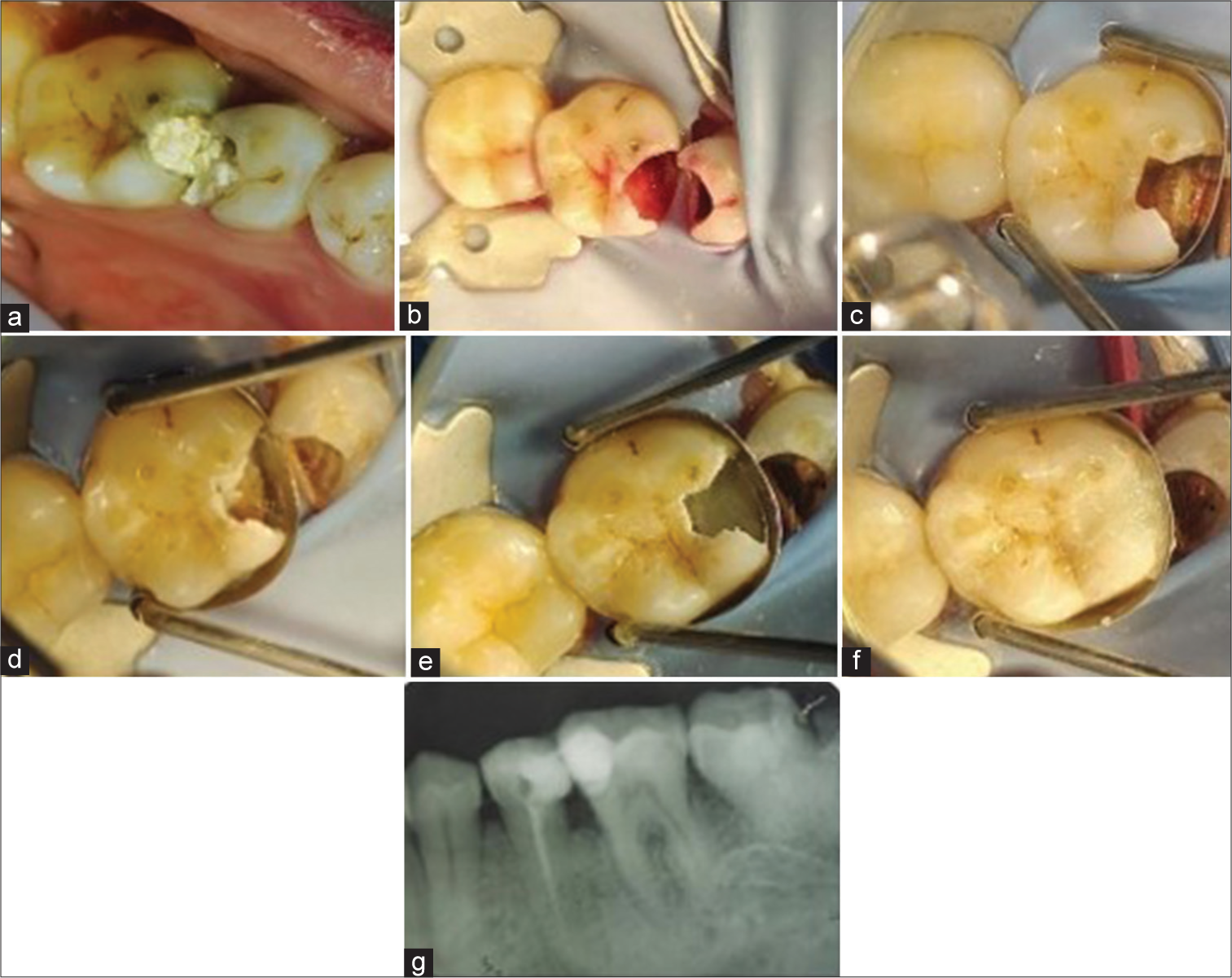
- (a) Pre-operative clinical image, (b) application of caries detection dye, and (c) on complete caries removal subgingival margin was seen with respect to 46. (d) Indirect pulp capping using MTA, (e) margin elevation done using RMGIC, (f) composite restoration done, and (g) post-operative radiograph showing endodontic treatment with respect to 45 and deep margin elevation followed by direct restoration with respect to 46. MTA: mineral trioxide; RMGIC: resin-modified glass ionomer cement.
Informed consent was taken from the patient. Oral prophylaxis was done before the commencement of treatment. A rubber dam was placed for isolation and protection of soft tissue from any possible chemical or mechanical injury. Gross caries removal was done with No. 2 round bur (Mani, India). One drop of caries detection dye (1% Acid Red solution in a propylene glycol solvent) was applied using a micro-brush and allowed to penetrate for 10 s, followed by which it was rinsed with water and then air dried. Complete caries excavation was done using diamond burs, and ultrasonic tips were used to clear off the debris and get clean margins. Pulpal exposure was noted, and bleeding was arrested using 5.25% sodium hypochlorite for 3 min. Once the bleeding was completely arrested, matricing was done using a pre-contoured sectional matrix (Tor Vm matrix, Filaydent, India). MTA (SafeEndo) was mixed according to manufacturer instructions and was placed at the site of pulpal exposure. Dentine conditioning was done using 10% phosphoric acid before placement of RMGIC. RMGIC (SafeEndo, India) was used for margin elevation. The restoration was done using dental composite resin (3M Filtek Z250 XT Nano Hybrid Universal Restorative cement). It was used as it is a nanocomposite having the advantage of better dimensional accuracy and mechanical properties.
At 1-year follow-up, gingival health was found to be satisfactory. A probing depth of 2 mm was seen with no bleeding on probing.
DISCUSSION
Preserving healthy tooth structures is one of the primary objectives of modern restorative dentistry. Thus, concepts and guidelines for minimum intrusive preparation are chosen.[5] The basis for DME is the coronal movement of the restorative margin rather than the displacement of the periodontium margin in accordance with the cavity limits.
The traditional method for treating subgingival defects involved either orthodontic extrusion or surgical exposure through crown lengthening. However, these procedures have a number of disadvantages, such as decreased esthetics, loss of attachment, hypersensitivity of the dentin, an unfavorable crown-to-root ratio, and exposure of the root concavities and furcations to the oral environment. Furthermore, this process may often cause a delay in the delivery of the final restoration.[4]
A rubber dam was used for isolation, circumferential stainless steel matrix was used. The dimensions of the matrix should be thin enough to allow for easy slipping in the subgingival area but yet higher than the desired elevation level. Due to this, it might need to be trimmed with scissors to a size of 2-3 mm. For the matrix to be stable, there must be enough tooth substance at the buccal and lingual walls. If this is not the case, the treatment plan needs to be reevaluated because instability equates to method failure. Between the cavity margin and the matrix, there should be no interference from gingival tissue or rubber dam.[4]
Three factors are critical for DME: biological width, matricing, and rubber dam isolation.
“Supracrestal tissue attachment” (STA) is the new term for “biological width;” it describes the apicocoronal dimension of gingival attachment adjacent to the root surface (junctional epithelium + supracrestal connective tissue). Standard STA measurements do not exist, and the primary source of variability (1–3 mm) is the epithelial attachment, whereas connective tissue height remains constant.[6] It is, therefore, impossible for the clinician to determine whether a deep subgingival lesion stays inside the epithelial attachment or invades the connective tissue. Ghezzi et al.[7] presented a novel classification system for deep proximal cavities based on rubber dam isolation capacity, independent of the size of the carious lesion.
Surgical intervention is deemed unnecessary when a rubber dam can be positioned, as it is presumed that the operating field is restricted within the epithelium area. Conversely, in the event of an invasion of connective tissue, it is technically impossible to separate the area, and surgical treatments are necessary.[7] Different supra-crestal attachment patterns were seen after the composite was placed subgingivally. The material could not form a connective attachment, as shown by a histological investigation.[3] Therefore, it is imperative to emphasize that the long junctional epithelium serves as the sole pathway for achieving periodontal attachment to the substrate.
In DME, a range of materials and techniques are used, including several matrix systems. A single Tofflemire band or one modified by a sectional matrix embedded therein, with Teflon tape placed apically in between the matrices (the M-i-M approach). Sectional matrices that have been modified using Teflon tape can be utilized, and Reel Matrix (Garrison, MI, USA) has been designed.[8]
Marginal integrity: Indirect composite restorations generally result in less polymerization shrinkage compared to direct restorations, making them a preferable option. Roggendorf et al.[9] conducted an in vitro study to investigate how DME affects the marginal integrity of resin composite inlays. They used scanning electron microscopy to evaluate the marginal integrity, finding that multiple layers of DME performed better than single-layer applications. In addition, bonding inlays to dentin with unraised margins resulted in fewer gaps compared to DME applications. Da Silva et al.[10] found that universal adhesives were more effective in sealing cavities with dentin margins compared to ERAs. However, when the edges were placed on enamel, improved sealing was noted regardless of the adhesive type used.
Fracture resistance: Ilgenstein et al.[11] investigated the impact of DME and various materials on the fracture resistance of teeth restored with CAD/CAM ceramic and composite onlays. Their findings indicated that DME does not influence fracture resistance, regardless of the material used. This conclusion aligns with Grubbs et al.,[12] who found no statistically significant difference in fracture resistance among margins treated with bulk-fill composites, glass ionomers, or resin-modified glass ionomers after loading. Similarly, Bresser et al. studied the effect of preparation design and DME on the fracture resistance of CAD/CAM lithium disilicate ceramic crowns and reported that DME did not significantly affect fracture resistance.[13]
Technique plays a critical role in direct restorative bonding, especially when it involves areas beneath the cementum or enamel margins. The absence of enamel at cervical margins creates a weak spot for effective bonding, potentially threatening the integrity of the tooth’s margins. Cervical enamel is thinner, less organized, and features a more dense, less structured arrangement compared to the more orderly prismatic enamel found in mid-coronal regions. This difference in structure results in shorter resin tags and diminished bond strength, affecting the long-term durability of the bond. In addition, the presence of cementum at subgingival margins further compromises the effectiveness of the adhesion. [14]
We opted to do DME as the restorative margin was extending subgingivally, and proper isolation was possible; the most conservative approach of DME along with fiber post and core was used in the first case, and pulp protection using MTA and direct composite restoration was used in the second and third case.
CONCLUSION
DME is a promising method that conservatively repositions the cervical margin coronally, allowing cementation, impression-taking, and field isolation. DME can be employed in both direct and indirect restorations. The majority of the published literature focuses on in vitro research. Consequently, to elucidate every facet of the methodology and determine its efficacy in clinical settings, randomized clinical studies featuring prolonged observation periods are required. DME should be used cautiously for the time being, taking into account three factors: the ability to isolate the field, the matrix’s perfect sealing of the cervical margin, and the no biological width connective tissue invasion.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodont Aesthet Dent. 1998;10:47-54.
- [Google Scholar]
- Deep margin elevation versus crown lengthening: Biologic width revisited. Int J Esthet Dent. 2018;13:334-56.
- [Google Scholar]
- Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz Oral Res. 2018;32:e74.
- [CrossRef] [Google Scholar]
- Biologic width dimensions-a systematic review. J Clin Periodontol. 2013;40:493-504.
- [CrossRef] [Google Scholar]
- Cervical margin relocation: Case series and new classification system. Int J Esthet Dent. 2019;14:272-84.
- [Google Scholar]
- Deep margin elevation in restorative dentistry: A scoping review. J Dent. 2024;146:105066.
- [CrossRef] [Google Scholar]
- Effect of proximal box elevation with resin composite on marginal quality of resin composite inlays in vitro. J Dent. 2012;40:1068-73.
- [CrossRef] [Google Scholar]
- Influence of the adhesive strategy in the sealing ability of resin composite inlays after deep margin elevation. J Clin Exp Dent. 2021;8:e886-93.
- [CrossRef] [Google Scholar]
- Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin Oral Investig. 2014;19:1021-8.
- [CrossRef] [Google Scholar]
- Efficacy of direct restorative materials in proximal box elevation on the margin quality and fracture resistance of molars restored with CAD/CAM onlays. Oper Dent. 2020;45:52-61.
- [CrossRef] [Google Scholar]
- Influence of deep margin elevation and preparation design on the fracture strength of indirectly restored molars. J Mech Behav Biomed Mater. 2020;110:103950.
- [CrossRef] [Google Scholar]
- Deep proximal margin rebuilding with direct esthetic restorations: A systematic review of marginal adaptation and bond strength. Restor Dent Endod. 2022;47(2)
- [CrossRef] [Google Scholar]






